Ear Infection Treatment Online
Stop ear pain and discomfort fast. See an online doctor for expert treatment of ear infections tailored to your needs.
Available in 50 states. Insurance accepted.
Fast
virtual visits
24/7 care
assistants
Prescriptions
as needed

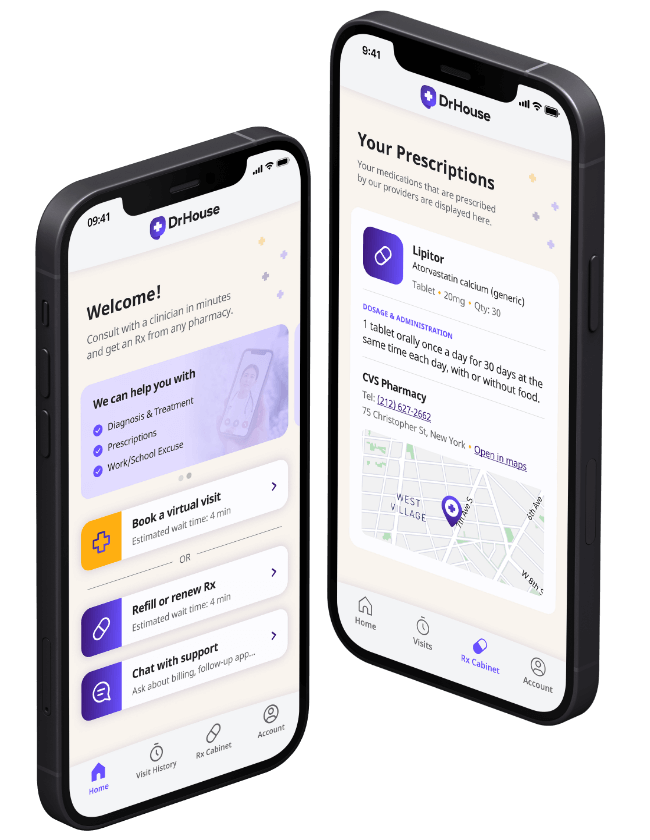
24/7 Personal Care
Consult with a physician in 15 minutes, refill an Rx or chat with our care assistants.

Affordable & Convenient
See your cost upfront and get treatment for hundreds of different conditions.

Insurance Accepted
We accept most major insurance plans, making healthcare easy and affordable.
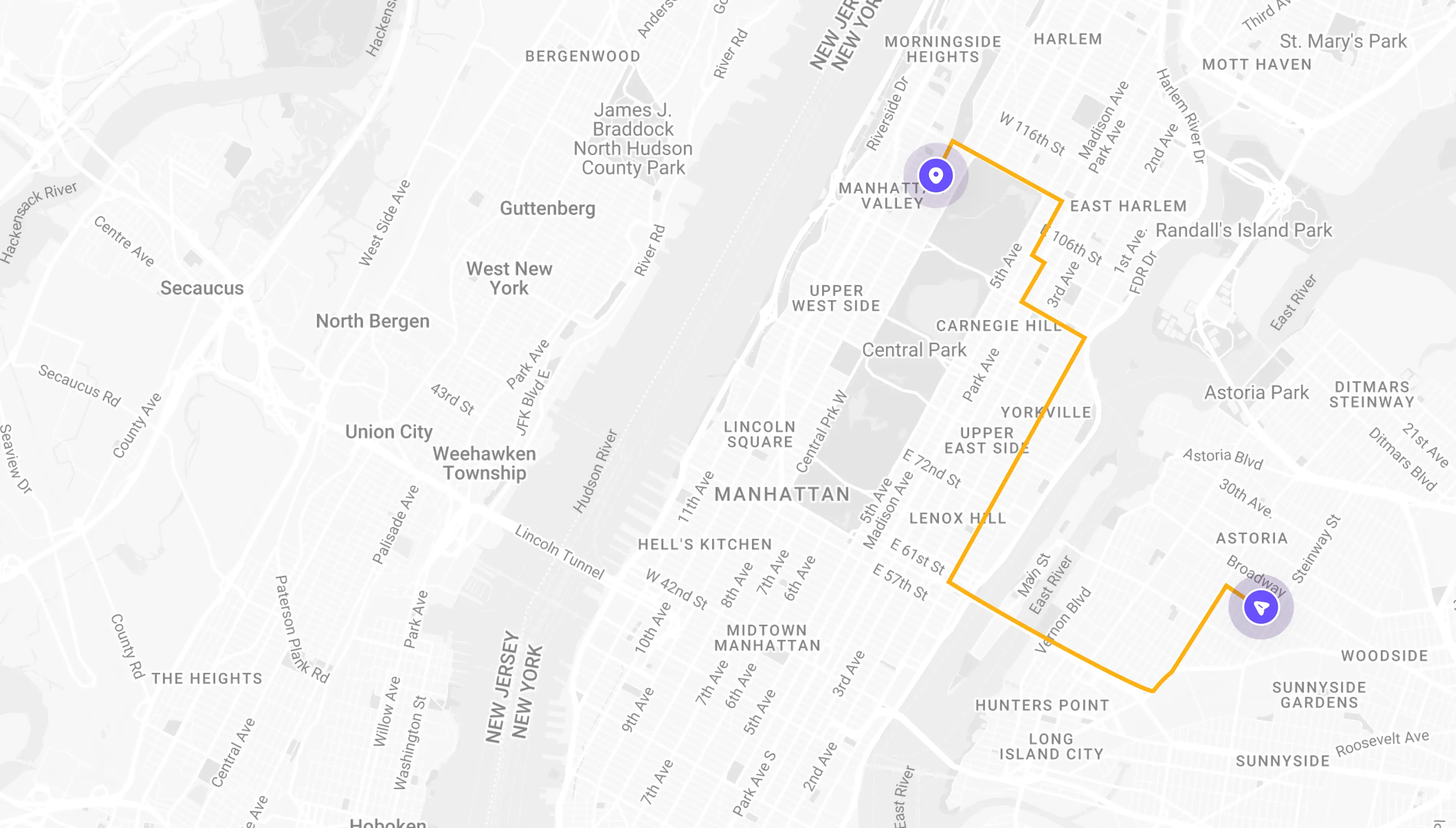
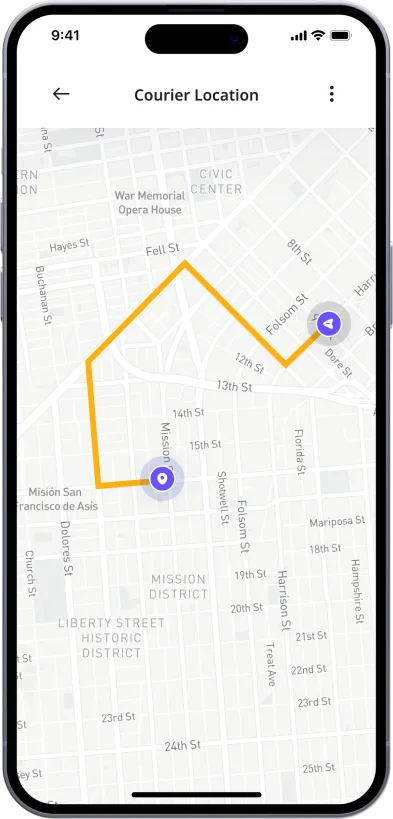
See If Delivery Is Available Near You
Delivery Not Available
Enter your ZIP code to check if prescription delivery is available in your area and how soon your meds could arrive.
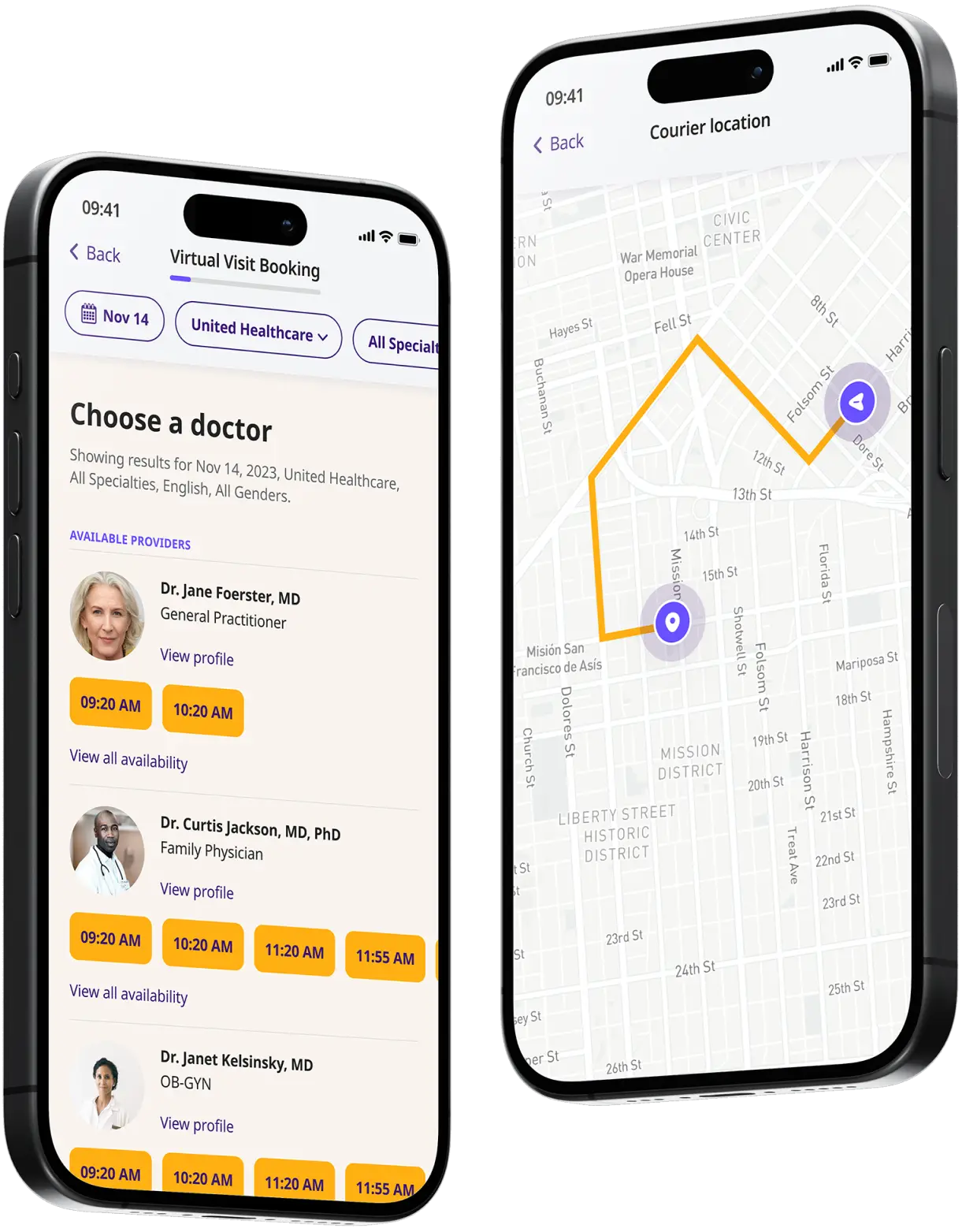
How to get started
Choose your doctor, start a virtual visit, and have your prescriptions sent to your preferred pharmacy for pickup — all in just a few easy steps.
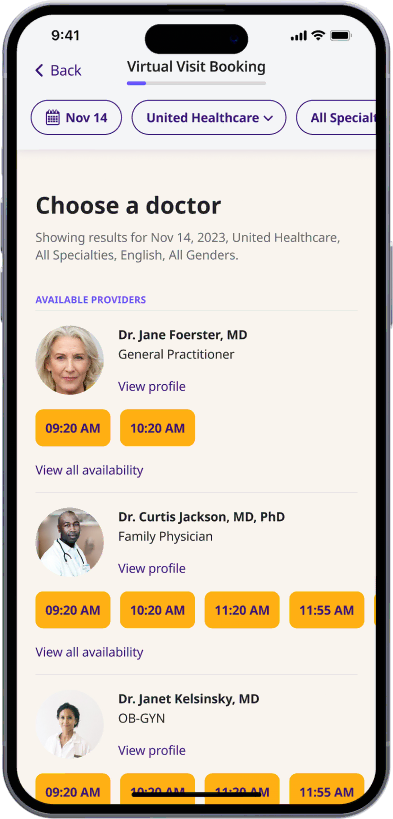
Choose a doctor
Choose a physician by availability, specialty, ratings, and more.
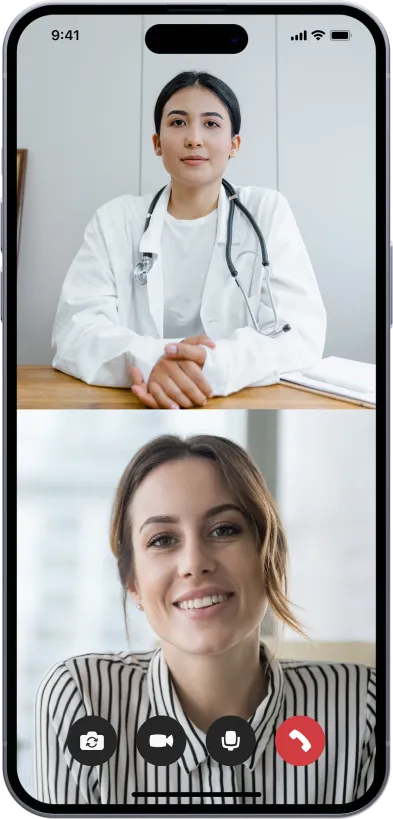
Start your video visit
Connect with a doctor in minutes on a secure video call.
Get your prescription
Pick up your meds or have them delivered in as little as an hour.
Available in 50 states. Insurance accepted.
One-Time
Physician Visit
One-time visit with a physician for diagnosis, treatment, Rx, labs, referrals, and doctor’s notes.
Accepted Insurances
See why people turn to DrHouse...
As seen in

Ear Infection Treatment Online
Ear infections are common conditions that can affect anyone, though they are particularly prevalent among children. An ear infection occurs when a bacterial or viral infection affects the middle ear, the section just behind the eardrum.
The infection often results in pain, fluid buildup, and inflammation. Depending on the part of the ear that is infected, ear infections are classified into three main types: middle ear infection (acute otitis media), inner ear infection (labyrinthitis), and outer ear infection (otitis externa).
Each type of ear infection has distinct causes, symptoms, and treatment approaches. Some ear infections resolve on their own and are managed effectively with pain relief methods and home remedies, while others may require medical intervention including antibiotics or even surgical procedures in severe cases.
Middle ear infection (acute otitis media)
Middle ear infection, or acute otitis media, is the most frequent type of ear infection, especially among children. This condition occurs when bacteria or viruses from the nose and throat get trapped behind the eardrum, typically during or after a cold, flu, or respiratory infection. The infection causes an accumulation of pus and fluid behind the eardrum, leading to pain, fever, and in some cases, hearing loss.
The eustachian tubes, smaller and more horizontal in children than in adults, are often blamed for the prevalence of this condition in younger populations as they can easily get blocked.
Symptoms to watch for include severe ear pain, difficulty sleeping, hearing difficulties, fluid drainage from the ear, and irritability in children. Treatment generally involves pain management and monitoring the condition, but if symptoms persist or worsen, antibiotics may be prescribed to combat the infection.
Inner ear infection (labyrinthitis)
Labyrinthitis, commonly referred to as an inner ear infection, involves the inflammation of the inner ear or the nerves that connect the inner ear to the brain. This condition can cause severe symptoms, including vertigo (a spinning sensation), hearing loss, nausea, and balance disruption. These symptoms occur because the inner ear is responsible for both hearing and balance.
Labyrinthitis is usually caused by a viral infection but can also develop as a result of bacterial infections or, less commonly, as a complication of middle ear infection.
The treatment of labyrinthitis focuses on alleviating symptoms and may include medications to reduce nausea and manage vertigo. Corticosteroids may also be used to reduce inflammation, and antibiotics are prescribed if a bacterial infection is suspected. Recovery times vary, but many patients see improvements within several weeks.
Outer ear infection (otitis externa)
Otitis externa, more widely known as swimmer’s ear, is an infection of the outer ear canal running from the eardrum to the outside of the head. It often arises from water that remains in the ear after swimming, creating a moist environment that aids bacterial growth. It can also be caused by putting fingers, cotton swabs, or other objects in the ears, which can damage the thin layer of skin lining the ear canal.
Symptoms of otitis externa include ear pain, itching in the ear canal, redness inside the ear, and mild to moderate fluid drainage. In severe cases, the ear canal may swell shut or become blocked by debris or fluid, causing significant pain and hearing impairment.
Treatment typically involves keeping the ear dry, avoiding swimming, and using ear drops prescribed to reduce pain and inflammation. If the infection is severe or persistent, oral antibiotics may be needed.
What causes ear infections?
Ear infections result from either a viral or bacterial infection that affects one of the three parts of the ear—middle, inner, or outer.
The primary cause of these infections typically relates to inflammation and fluid buildup in the eustachian tubes, which connect the middle ear to the throat and nose. This can disrupt normal drainage and create an environment conducive to the growth of pathogens.
Here are some common factors that contribute to the development of ear infections:
- Common colds and respiratory infections: Viruses from the common cold or respiratory infections can spread to the eustachian tubes and middle ear, leading to acute otitis media. These conditions increase mucus production, inflammation, and swelling, which can block drainage pathways and allow fluids to accumulate in the middle ear.
- Allergies: Allergic reactions can cause similar effects in the ear as respiratory infections. Allergies often lead to swollen eustachian tubes and excessive mucus production, which can result in fluid buildup and subsequently, infections.
- Sinus infections: Sinus infections can cause increased mucus and inflammation, which may block the eustachian tubes and lead to secondary ear infections.
- Poor eustachian tube function: The eustachian tubes regulate air pressure and drain fluid from the middle ear. Some individuals, especially children, have eustachian tubes that do not function well due to their size, angle, or because they become easily clogged.
- Smoking and secondhand smoke: Exposure to tobacco smoke can irritate the eustachian tubes and increase the risk of ear infections.
- Climatic factors: Environmental factors such as high humidity and exposure to excessive moisture (like from swimming) can lead to outer ear infections, also known as swimmer’s ear.
- Physical injury or pressure changes: Injuries to the ear or pressure changes (experienced during flying or diving) can affect the ear’s ability to equalize pressure, leading to potential infections.
Risk factors for ear infections
Ear infections can affect anyone but are particularly common in young children. There are several factors that increase the risk of developing an ear infection. Understanding these risk factors can help in taking preventive measures and recognizing potential symptoms early on. Here are some of the main risk factors associated with ear infections:
- Age: Young children are more susceptible to ear infections because their eustachian tubes are narrower and more horizontal, which makes them more difficult to drain and more likely to get clogged.
- Group child care: Children in group care settings are exposed to more infections at an early age due to increased contact with other children. This exposure can lead to more frequent colds and respiratory infections, increasing the risk of ear infections.
- Infant feeding practices: Babies who are bottle-fed, especially while lying down, have a higher risk of ear infections compared to those who are breastfed. Breastfeeding provides antibodies that help to protect against early infections, including those that can lead to ear infections.
- Seasonal factors: Ear infections are more common during the fall and winter when colds and flu are prevalent. People tend to spend more time indoors, which can increase the spread of viruses.
- Poor air quality and tobacco smoke: Exposure to tobacco smoke and polluted air can irritate the eustachian tubes, impairing their function and increasing the risk of ear infections.
- Allergies: Chronic allergies can lead to swelling and blockage of the eustachian tubes, which can contribute to the development of ear infections.
- Sinus infections: Ongoing sinus infections can cause or exacerbate ear infections by affecting the drainage of the eustachian tubes.
- Genetics: There is some evidence that a tendency to develop ear infections can be inherited, meaning that if ear infections are common in your family, there is a higher chance that you or your children might also be prone to them.
- Cleft palate or other craniofacial abnormalities: Structural abnormalities in the skull or facial structure can affect the function of the eustachian tubes and increase the risk of ear infections.
- Immune deficiencies: Individuals with weakened immune systems, either from immune disorders or from treatments like chemotherapy, are at higher risk for infections, including ear infections.
Ear infection symptoms
Ear infection symptoms can vary depending on the type of infection (middle, inner, or outer ear infection) and the severity. Recognizing these symptoms is crucial for timely and effective treatment. Here’s a breakdown of the common symptoms associated with each type of ear infection:
Middle ear infection (acute otitis media)
Symptoms of a middle ear infection often appear quickly and include:
- Ear pain: This is often severe and worsens when lying down as pressure changes in the ear.
- Tugging at the ear: Young children who cannot express their pain may tug or pull at their ears.
- Difficulty sleeping: Pain often worsens at night, making it hard to sleep.
- Hearing problems: Fluid buildup can cause noticeable hearing difficulties.
- Fluid drainage: You may observe pus or fluid leaking from the ear.
- Fever: Especially common in children, a fever over 100.4°F (38°C) can accompany an ear infection.
- Irritability and crying: In infants and toddlers, increased crying and irritability are common signs.
Inner ear infection (labyrinthitis)
Symptoms of inner ear infections include:
- Vertigo: A spinning sensation that can be severe and may cause nausea or vomiting.
- Imbalance or difficulty walking: Disruption in balance makes it hard to stand or walk without support.
- Nausea and vomiting: Often accompanied by vertigo.
- Hearing loss: Can be sudden or progressive.
- Tinnitus: Ringing or buzzing sounds in the ear.
- Ear pain: Not as common as with middle ear infections, but can occur.
Outer ear infection (otitis externa)
Commonly known as swimmer’s ear, symptoms include:
- Ear pain: Pain that intensifies when the outer ear is touched or pulled.
- Itching in the ear canal: Often the first symptom.
- Redness in the ear: Visible irritation and redness in the outer ear.
- Swelling of the ear canal: Makes the ear feel full, and may affect hearing.
- Discharge: Pus or fluid drainage, which might be clear, white, yellow, or even greenish.
- Lymph node swelling: Nearby lymph nodes may swell and become tender.
These symptoms can significantly affect the quality of life, particularly if they are severe or persistent. If you or your child experiences any of these symptoms, particularly with severe pain, fever, or ongoing hearing loss, it’s important to seek medical attention promptly.
Early intervention can prevent complications, alleviate discomfort, and expedite recovery.
Treatment for ear infections
Treatment for ear infections varies based on the type of infection and its severity. Management strategies range from watchful waiting to medical interventions, including medications and, in some cases, surgery. Here’s an overview of the treatment options for different types of ear infections:
Middle ear infections (acute otitis media)
For middle ear infections, treatment options include:
- Watchful waiting: Many mild cases of acute otitis media may resolve without antibiotic treatment, especially in children over two years old who have mild symptoms. During this period, pain can be managed with over-the-counter pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil).
- Antibiotics: If symptoms are severe or do not improve within 48-72 hours, or if the patient is a young child or has a high fever, antibiotics may be prescribed. Amoxicillin is often the first choice.
- Ear drops: In cases with tympanostomy tubes or where there’s a perforation in the eardrum, antibiotic ear drops may also be used.
- Pain management: Pain relievers are often recommended to alleviate ear pain associated with infections.
Inner ear infections (labyrinthitis)
Treatment of inner ear infections focuses on relieving the symptoms:
- Medications for nausea and vertigo: Drugs such as meclizine, promethazine, or diazepam can help control vertigo and nausea.
- Steroids: To reduce inflammation within the inner ear.
- Antibiotics or antivirals: These are used if a bacterial infection or a viral infection is identified as the cause.
- Bed rest: Keeping still can help reduce the sensation of spinning and dizziness.
Outer ear infections (otitis externa)
For outer ear infections, treatment typically involves:
- Ear drops: Antibiotic ear drops with or without steroids are the main treatment to fight infection and reduce inflammation.
- Pain relief: Over-the-counter pain relievers can help manage pain.
- Keeping the ear dry: It’s important to keep the ear canal dry during treatment. A plug or waterproof ear cover can be used during showering or bathing.
- Cleaning: Sometimes, if the ear canal is very swollen, a healthcare provider may need to clean out the ear canal.
- Oral antibiotics: These are reserved for more severe cases or if the infection spreads beyond the ear.
General care and management
- Heat compresses: Applying a warm compress to the affected ear can help relieve discomfort.
- Hydration and rest: Adequate fluids and rest are important to help the body fight off infection.
- Avoiding ear insertion: Do not insert cotton swabs, fingers, or any objects into the ear, as this can aggravate the condition.
Ear infection medication
Effective treatment of ear infections often involves the use of medications to relieve pain and combat infections. The choice of medication depends on the type of ear infection and the severity of symptoms. Here’s a detailed look at common medications used to treat different types of ear infections:
Middle ear infections (acute otitis media)
For middle ear infections, the following medications are commonly prescribed:
- Antibiotics: If symptoms are severe or do not improve within a few days, antibiotics may be necessary. The most commonly prescribed antibiotic for middle ear infections is Amoxicillin. For patients allergic to penicillin, alternatives like Azithromycin or Clarithromycin may be used.
- Pain relievers: Over-the-counter pain relievers like Acetaminophen (Tylenol) and Ibuprofen (Advil, Motrin) are recommended to manage pain and reduce fever. These medications can help make patients more comfortable while the infection resolves.
Inner ear infections (labyrinthitis)
Treatment for inner ear infections may include:
- Corticosteroids: Such as Prednisone, Middle-rarreduce inflammation in the inner ear.
- Antiviral or antibacterial medications: Depending on whether the infection is viral or bacterial, medications such as valacyclovir (for viral infections) or oral antibiotics (for bacterial infections) may be prescribed.
- Medications for nausea and dizziness: Drugs like Meclizine, Promethazine, or Diazepam can help alleviate symptoms of vertigo and nausea associated with inner ear infections.
Outer ear infections (otitis externa)
For outer ear infections, commonly known as swimmer’s ear, treatment typically involves:
- Ear drops: Antibiotic ear drops are the primary treatment for reducing infection and inflammation. Drops may contain antibiotics such as Ofloxacin or Ciprofloxacin and often include a steroid like Hydrocortisone to reduce swelling.
- Oral antibiotics: In cases where the infection is severe or there is spreading beyond the ear, oral antibiotics may be necessary.
Prevention
Preventing ear infections is particularly crucial for reducing discomfort, minimizing the need for medical treatment, and avoiding recurrent infections, especially in children who are more susceptible. Here are several effective strategies to help prevent ear infections:
- Hand washing: Regular hand washing is one of the most effective ways to prevent the spread of infections that can lead to ear infections.
- Avoid smoke exposure: Tobacco smoke can irritate the eustachian tubes and increase the risk of ear infections. Ensure that environments are smoke-free, especially around children.
- Maintain good overall health: Strengthening the immune system through a balanced diet, adequate sleep, and regular physical activity can help resist infections.
- Breastfeeding: Breastfeeding for at least six months can help provide antibodies that protect against early childhood infections, including ear infections.
- Bottle feeding position: If bottle feeding, hold your child in an upright position rather than lying down to prevent milk from entering the eustachian tubes, which can contribute to ear infections.
- Vaccinations: Ensure children are up-to-date on vaccinations, including the pneumococcal vaccine and the flu vaccine, which can help prevent infections that may lead to ear infections.
- Allergy management: If you or your child has allergies, managing them with the help of a healthcare provider can prevent the allergic reactions that contribute to ear infections.
- Treat colds and flu promptly: Reducing the duration and severity of colds and flu can help prevent the complications that lead to ear infections.
- Dry ears thoroughly: After swimming or bathing, dry the ears thoroughly with a towel or hair dryer on a low setting held at a distance. This helps prevent moisture in the ear canal, which can lead to infections.
- Avoid inserting objects in your ears: Cotton swabs, fingers, and other objects should not be inserted into the ears, as they can damage the skin in the ear canal and provide a gateway for bacteria.
- Humidity control: Use a dehumidifier in damp environments to help prevent the growth of bacteria and fungi in the home.
- Water protection: Use earplugs or custom-fitted swim molds when swimming to prevent water from getting trapped in the ear canal, especially if you are prone to ear infections.
- Regular check-pps: Especially for children, regular check-ups can help catch and address potential issues before they turn into infections.
How can DrHouse help you?
DrHouse is a telehealth platform that offers a convenient and effective way to manage and treat ear infections from the comfort of your home. The service provides a range of healthcare solutions tailored to the needs of individuals experiencing ear-related issues. Here’s how DrHouse can assist you in dealing with ear infections:
- Online consultations: DrHouse allows you to consult with qualified healthcare providers via video calls or chat, enabling timely diagnosis and treatment recommendations without the need to visit a doctor’s office.
- Flexible scheduling: Appointments can be scheduled at times that suit your lifestyle, including evenings and weekends, ensuring you can get help when you need it most.
- Personalized care: Based on your symptoms and medical history, DrHouse doctors can develop a personalized treatment plan that may include prescriptions, lifestyle adjustments, and preventive measures.
- Nationwide access: DrHouse services are available across the entire United States, ensuring that you can access quality healthcare regardless of your location.
- No need for insurance: While DrHouse accepts a variety of insurance plans, services are also accessible without insurance, which can be particularly beneficial for those with limited coverage.
DrHouse leverages the convenience of modern technology to provide comprehensive, patient-centered care for ear infections and other health issues.
Whether you need a quick consultation for sudden ear pain or require ongoing management for recurrent issues, DrHouse is designed to meet your health needs effectively and efficiently.
Frequently asked questions (FAQs)
Can an ear infection be treated online?
Yes, ear infections can be diagnosed and treated online through the use of telehealth services such as DrHouse. The online doctors at DrHouse can diagnose, provide treatment recommendations, and even prescribe medication if necessary.
Is it safe to get treatment for an ear infection without physically visiting a doctor’s office?
Yes, with the advancement of technology and qualified healthcare providers on telemedicine platforms like DrHouse, it is safe to receive treatment for ear infections without leaving your home. However, if symptoms persist or worsen, it is important to seek in-person medical attention.
Can I get a prescription for ear infection medication from DrHouse?
Yes, if deemed necessary by the online doctor during your consultation, DrHouse can facilitate a prescription for ear infection medication.
Frequently asked questions