Get UTI Treatment and Antibiotics Online
Get fast, effective UTI treatment and antibiotics online with 24/7 expert advice and personalized care from our virtual doctors.
Available in 50 states. Insurance accepted.
Fast
virtual visits
24/7 care
assistants
Prescriptions
as needed



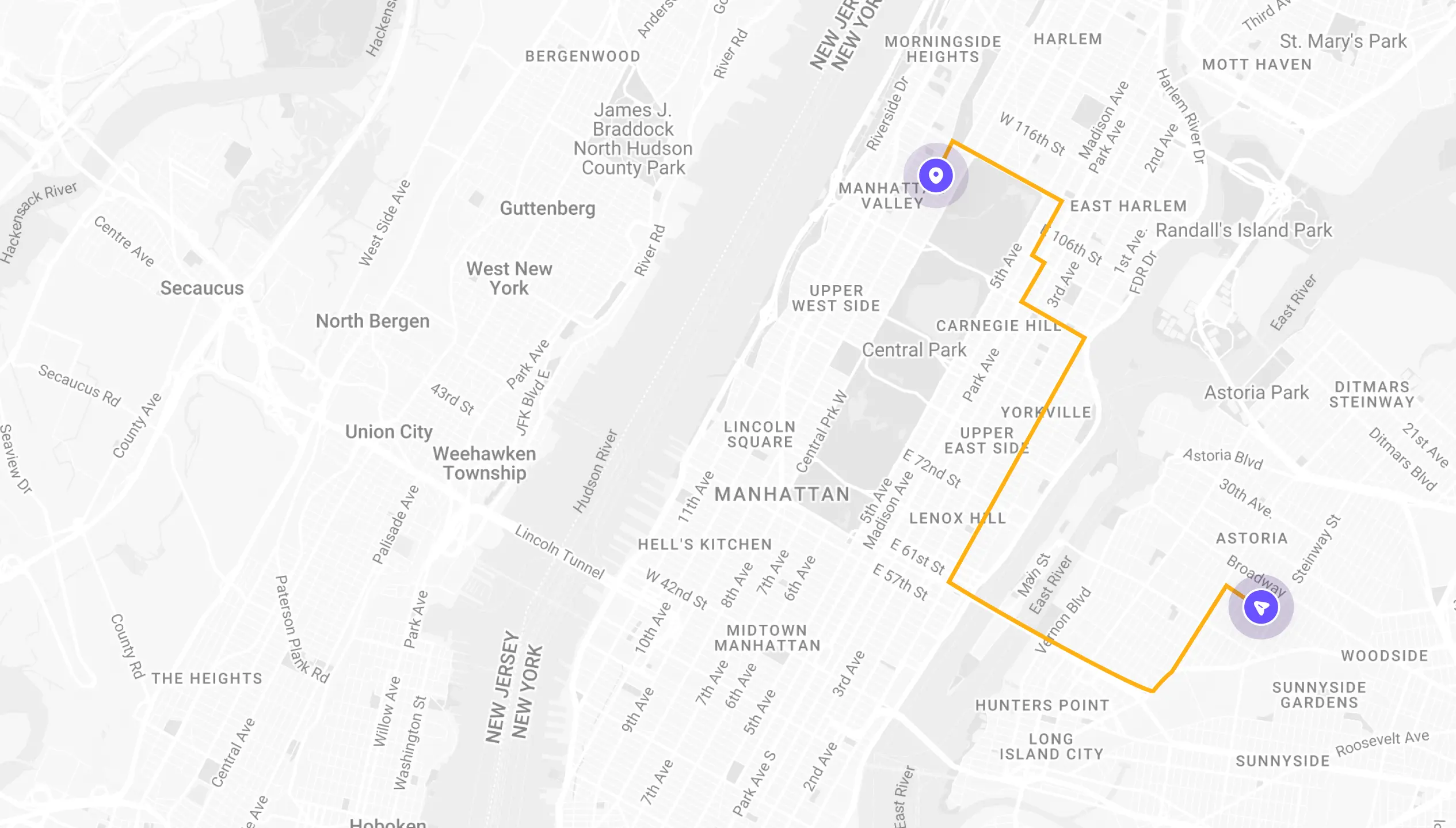
See If Delivery Is Available Near You
Delivery Not Available
Enter your ZIP code to check if prescription delivery is available in your area and how soon your meds could arrive.
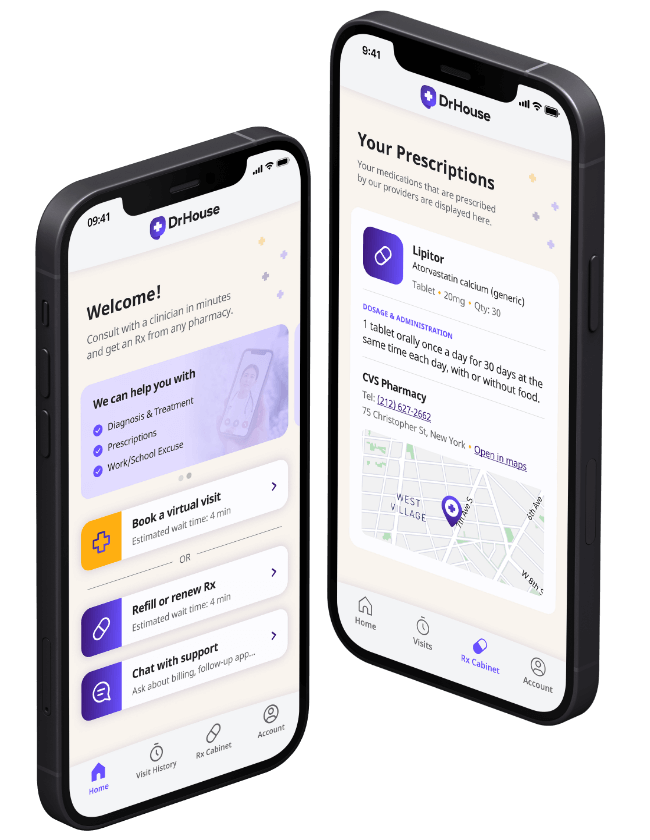
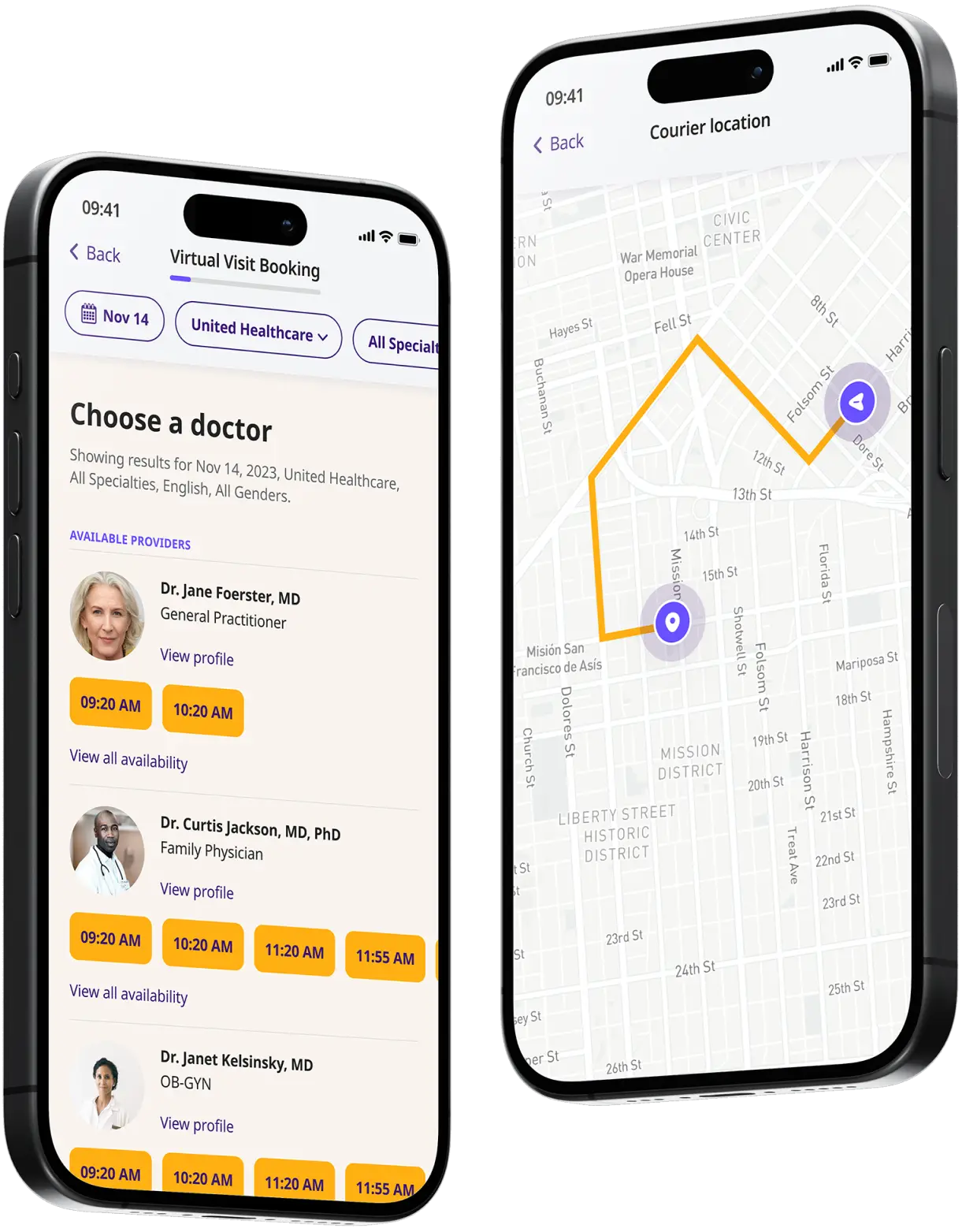
How to get started
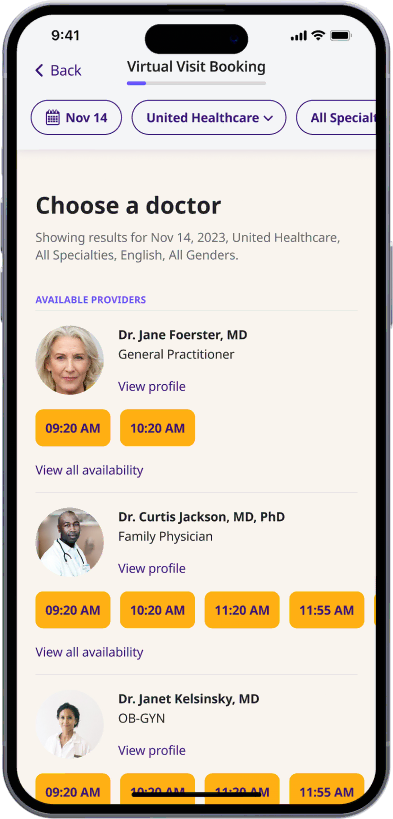
Choose your doctor, start a virtual visit, and have your prescriptions sent to your preferred pharmacy for pickup — all in just a few easy steps.
Choose a doctor
Choose a physician by availability, specialty, ratings, and more.
Start a video call
Get connected with a doctor anytime, anywhere.
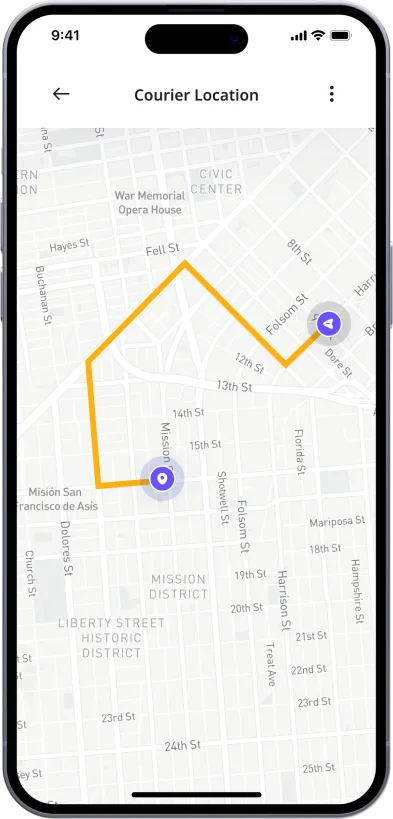
1-Hour Rx Delivery
Your prescription delivered to your door in 1 hour or less.
Available in 50 states. Insurance accepted.
One-Time
Physician Visit
One-time visit with a physician for diagnosis, treatment, Rx, labs, referrals, and doctor’s notes.
Accepted Insurances
See why people turn to DrHouse...
As seen in

Online UTI Treatment and Antibiotics
What is a UTI?
UTI stands for Urinary Tract Infection. It is an infection that can occur in any part of the urinary system, including the kidneys, ureters, bladder, and urethra.
UTIs are relatively common, affecting around 1 in 2 women and 1 in 20 men at some point in their lives. Women are more prone to UTIs because they have a shorter urethra, which makes it easier for bacteria to travel from the outside of the body to the bladder. People who are pregnant, have diabetes, or have a weakened immune system are also at increased risk for developing a UTI.
If left untreated, a UTI can lead to serious complications, such as kidney damage. For most people, however, a UTI can be effectively treated with antibiotics.
Types of UTIs
There are three main types of UTI: cystitis, urethritis, and pyelonephritis.
- Cystitis is an infection of the bladder that is characterized by pain and burning during urination, cloudy urine, and a strong urge to urinate.
- Urethritis is an infection of the urethra that is characterized by pain during urination, cloudy urine, and discharge from the penis or vagina.
- Pyelonephritis is an infection of the kidneys that is characterized by fever, chills, back pain, nausea, and vomiting.
What causes a UTI?
A urinary tract infection (UTI) is caused by bacteria that enter the urinary tract. The most common bacteria that cause UTIs include:
- Escherichia coli (E. coli)
- Klebsiella
- Proteus
- Pseudomonas
- Staphylococcus saprophyticus
UTI symptoms
A urinary tract infection (UTI) can cause a variety of symptoms, depending on the location of the infection and its severity. The most common symptom is a burning sensation when urinating. Other symptoms may include:
- frequently and urgently needing to urinate
- incontinence
- cloudy urine
- blood in the urine
- strong or foul-smelling urine
- pain in the side, abdomen, or pelvic area
- pressure in the lower pelvis
If the infection spreads to the kidneys, it can cause more severe symptoms such as fever, chills, and nausea.
UTI risk factors
- Female anatomy: Women are at a greater risk for UTIs than men. This is primarily because the length of the urethra is shorter in women, which leaves a shorter distance for bacteria to travel to get to the bladder. Also, the urethra is closer to the anus in women, which makes it easier for bacteria that linger around the anus, such as E. coli, can easily travel to the urethra.
- Being sexually active: Sexual activity can increase the risk of UTIs in women. During intercourse, bacteria from the genital area can be pushed into the urethra, leading to infections. Regular urination before and after sexual activity can help flush out any introduced bacteria and reduce the risk.
- Diabetes: People with diabetes have a weakened immune system, which makes it harder for their bodies to fight off infections, including UTIs. Additionally, elevated blood sugar levels can promote bacteria growth.
- Pregnancy: Pregnant women are at increased risk for UTIs, particularly later in pregnancy. This is due to hormonal changes and the growing fetus that can put pressure on the bladder and urinary tract, preventing urine from completely emptying from the bladder, which creates a breeding ground for bacteria.
- Certain birth control methods: Women who use diaphragms as a form of birth control might be at a higher risk of UTIs, especially if they also use spermicidal agents. These agents can increase bacterial growth and alter the natural balance of organisms in the vagina.
- Enlarged prostate: In men, an enlarged prostate can prevent the bladder from emptying fully. Residual urine can provide an environment for bacteria to grow. The enlarged prostate can block the flow of urine, increasing the risk of infection.
- Menopause: After menopause, a decline in circulating estrogen can lead to changes in the urinary tract that make you more vulnerable to infections. The thinning of the urinary tract lining, reduced bladder elasticity, and alterations in the balance of the vaginal flora can contribute to increased UTI risk.
Each of these factors can increase the risk of UTI. It’s always important for individuals to be aware of their own risk factors and take preventive measures when possible.
How is a UTI treated?
UTIs are usually treated with antibiotics, which typically clear the infection within a few days. However, some people may experience recurrent UTIs that require long-term antibiotic therapy or other interventions.
Some over-the-counter UTI medication can also be used to alleviate the symptoms.
f you suspect you have a UTI, consult with a healthcare provider to receive prompt diagnosis and treatment. With DrHouse, you can get started right away with a convenient online consultation.
UTI antibiotics
The most common antibiotics used to treat UTIs are:
- Nitrofurantoin
- Trimethoprim/sulfamethoxazole
- Fosfomycin
- Cephalexin
- Ceftriaxone
Each of these antibiotics works by killing the bacteria that cause the infection. However, they all have different side effects and risks, so it’s important to talk to a doctor about which one is right for you.
How to prevent UTIs?
There are several things you can do to help prevent UTIs:
- Drink plenty of fluids. Water helps to flush out bacteria from the urinary system.
- Urinate when you need to. Holding in urine can allow bacteria to grow.
- Wipe from front to back after using the restroom. This helps to prevent bacteria from entering the urethra.
- Avoid using feminine hygiene products that can irritate the urethra. These include douches, perfumed sprays, and powders.
- Urinate after sexual intercourse. This helps to flush out any bacteria that may have entered the urinary system during sex.
- See your healthcare provider for regular checkups and screenings. This is especially important if you have diabetes or a weakened immune system.
Get your UTI treated online with DrHouse!
If you think you may have a UTI, DrHouse can help. We offer online consultations with licensed healthcare professionals who can diagnose and treat your UTI.
Our physicians will work with you to develop a treatment plan that is right for you. We can also provide you with an online prescription for UTI antibiotics if medically appropriate.
With DrHouse, there’s no need to wait in line at the doctor’s office. So get started now and feel better tomorrow!
The content on this page has been medically reviewed for accuracy and comprehensiveness by Amy Dougherty, FNP-BC, AGAC
Related services
Explore more of our services tailored to your needs and discover additional ways we can support your healthcare needs.
Frequently asked questions