Bacterial Vaginosis Treatment Online
24/7 expert advice and treatment from DrHouse online doctors.
Available in 50 states. Insurance accepted.
Fast
virtual visits
24/7 care
assistants
Prescriptions
as needed



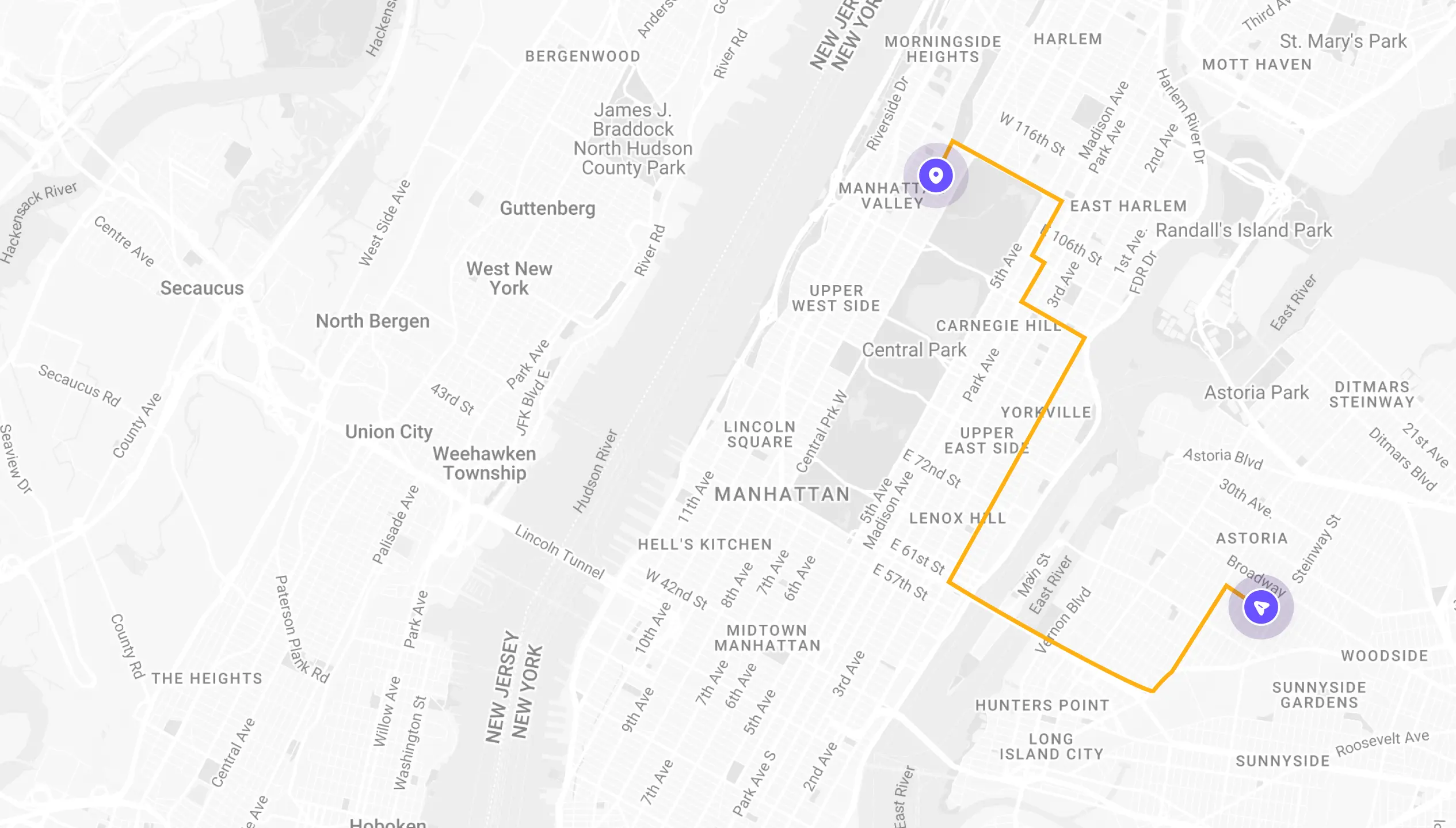
See If Delivery Is Available Near You
Delivery Not Available
Enter your ZIP code to check if prescription delivery is available in your area and how soon your meds could arrive.
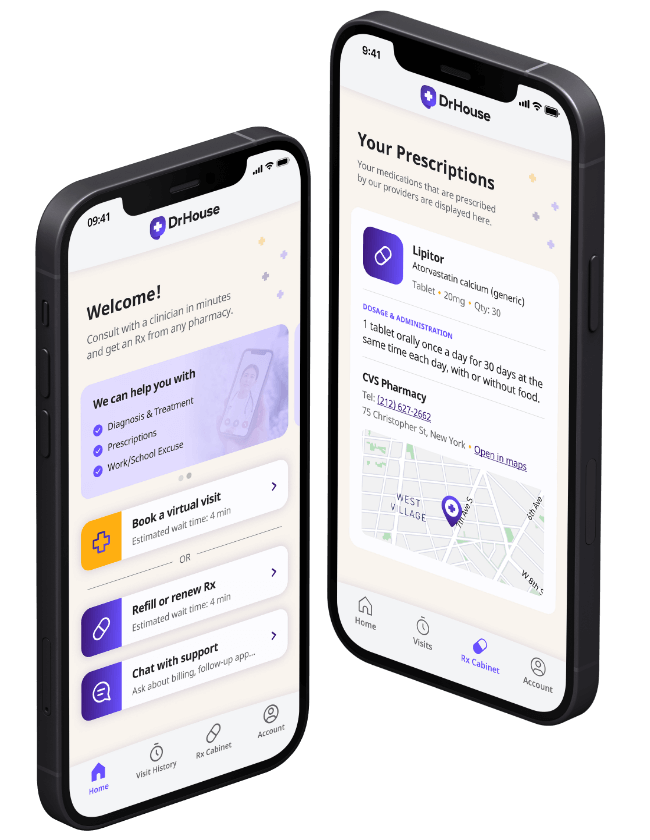
How to get started
Choose your doctor, start a virtual visit, and have your prescriptions sent to your preferred pharmacy for pickup — all in just a few easy steps.
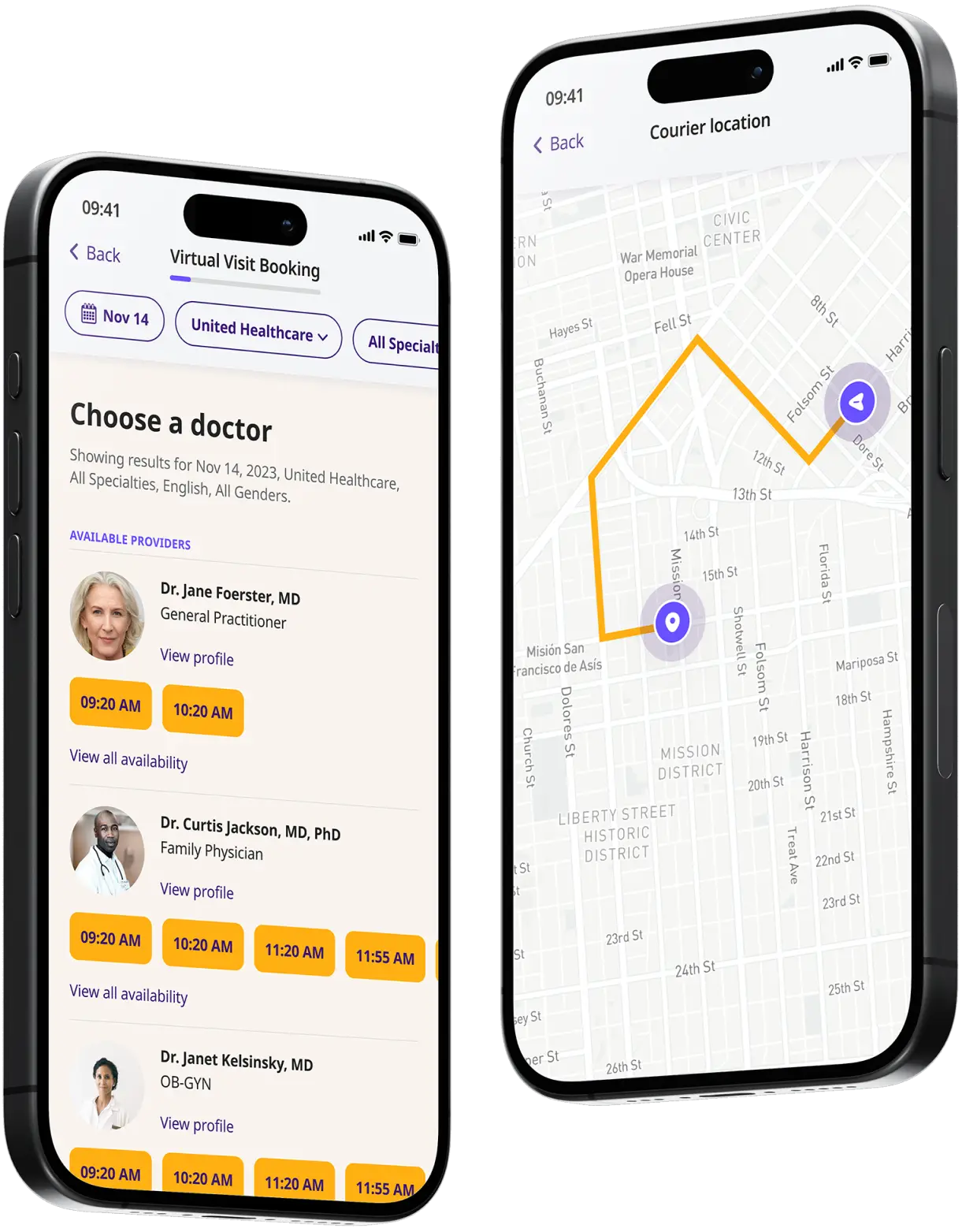
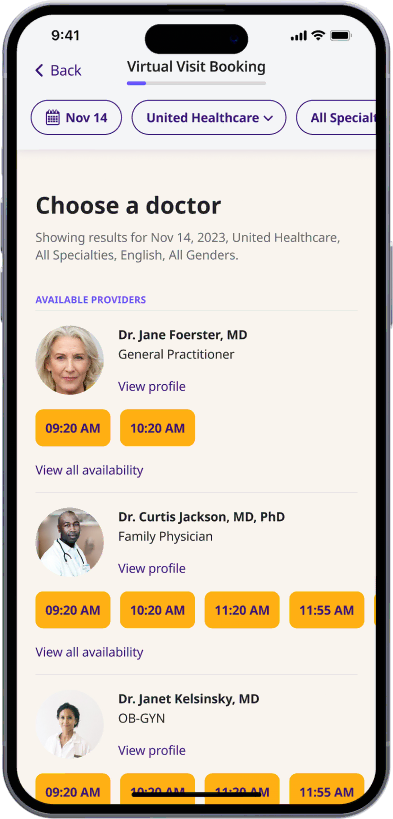
Choose a doctor
Choose a physician by availability, specialty, ratings, and more.
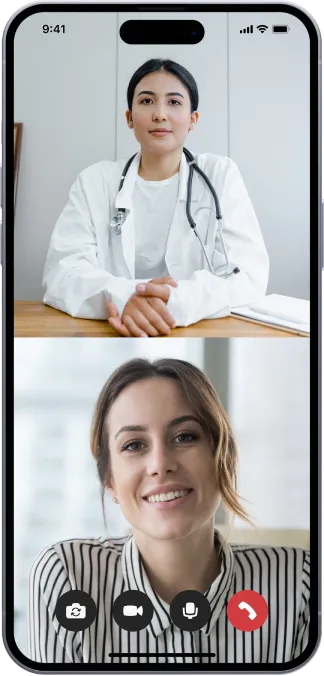
Start a video call
Get connected with a doctor anytime, anywhere.
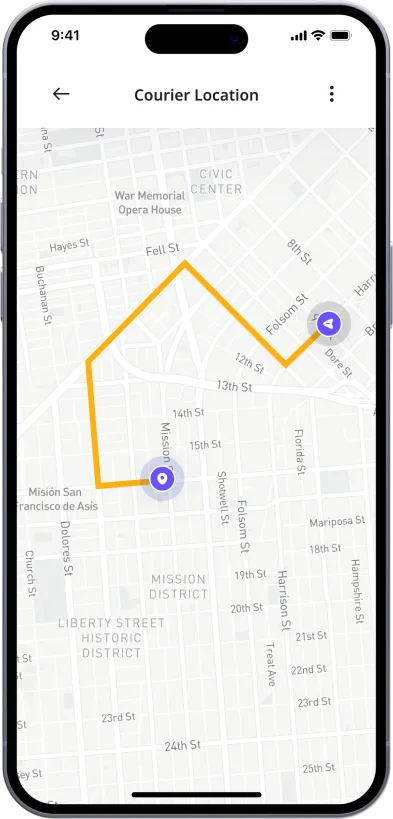
1-Hour Rx Delivery
Your prescription delivered to your door in 1 hour or less.
Available in 50 states. Insurance accepted.
One-Time
Physician Visit
One-time visit with a physician for diagnosis, treatment, Rx, labs, referrals, and doctor’s notes.
Accepted Insurances
See why people turn to DrHouse...
As seen in

About Bacterial vaginosis (BV)
What Is Bacterial Vaginosis (BV)?
Bacterial vaginosis (BV) is a type of vaginal infection caused by an overgrowth of bacteria. BV is the most common vaginal infection in women of childbearing age.
Although it may cause a number of uncomfortable and troubling symptoms (discharge, odor, itching), it is not generally considered a serious condition.
While BV is not considered a sexually transmitted infection (STI), it is often associated with sexual activity, and it can increase a woman’s risk of developing other STIs.
What Are the Symptoms of Bacterial Vaginosis (BV)?
Many women experience symptoms of Bacterial Vaginosis (BV) at some point in their lives. The most common symptoms include a fishy odor, burning, itching, and discomfort during urination or intercourse. Some women also experience a gray or white discharge. These symptoms can be mild or severe, and they may come and go.
BV symptoms include:
- White, gray, or even greenish vaginal discharge
- Thin, watery, or milky discharge
- Foul or “fishy” smelling vaginal odor
- Vaginal itching
- Burning feeling during urination
- Pain or discomfort during intercourse
- Sore or painful vagina
What Causes Bacterial Vaginosis?
Bacterial vaginosis is caused by an overgrowth of bacteria in the vagina. This can happen when there is a change in the pH balance or when the good bacteria that keep the vagina healthy are killed off.
Almost anything that disrupts the normal vaginal environment can lead to bacterial vaginosis, including:
- Douching
- Sexual activity
- Spermicides
- Antibiotics
- Having a new sexual partner
- Poor bathroom hygiene
- Pregnancy
How Is Bacterial Vaginosis (BV) Treated?
BV is treated with antibiotics, which can be taken orally or applied directly to the vagina in the form of a cream or gel.
In some cases, BV may resolve on its own without treatment. However, BV can increase the risk of other vaginal infections, such as yeast infections and sexually transmitted diseases (STDs), so it is important to see a doctor if you think you may have BV.
Common BV Prescription Medication
There are a number of different antibiotics that can be used to treat BV. The most common include metronidazole and clindamycin.
Other antibiotics used to treat BV include:
- Tinidazole
- Azithromycin
- Secnidazole
How Can DrHouse Help You?
At DrHouse, we offer bacterial vaginosis (BV) treatment online. Our online consultation and prescription service makes it easy to get the treatment you need from the comfort of your own home whenever you need it.
With our telehealth app, you can start on-demand online doctor visits in minutes, get diagnosed and receive a prescription for BV treatment – all from the convenience of your phone.
Our team of licensed medical professionals can help you identify the symptoms of BV and recommend the best course of treatment. We can also provide prescription medication for BV if needed.
So don’t wait – get started on your road to recovery today with DrHouse.
Frequently asked questions