Cellulitis Treatment Online
Treat cellulitis symptoms like redness and swelling quickly with online doctor visits—get expert care and prescriptions 24/7.
Available in 50 states. Insurance accepted.
Fast
virtual visits
24/7 care
assistants
Prescriptions
as needed

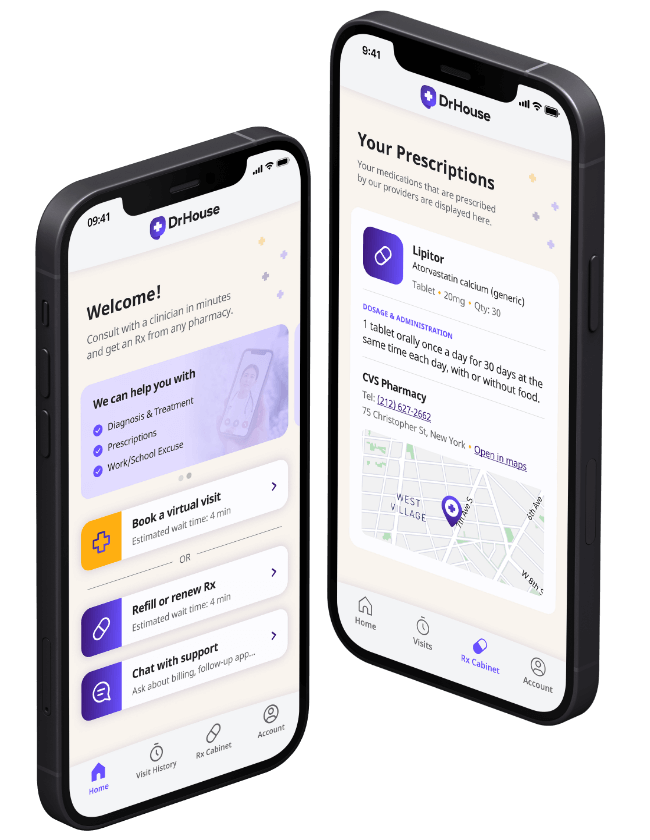
24/7 Personal Care
Consult with a physician in 15 minutes, refill an Rx or chat with our care assistants.

Affordable & Convenient
See your cost upfront and get treatment for hundreds of different conditions.

Insurance Accepted
We accept most major insurance plans, making healthcare easy and affordable.
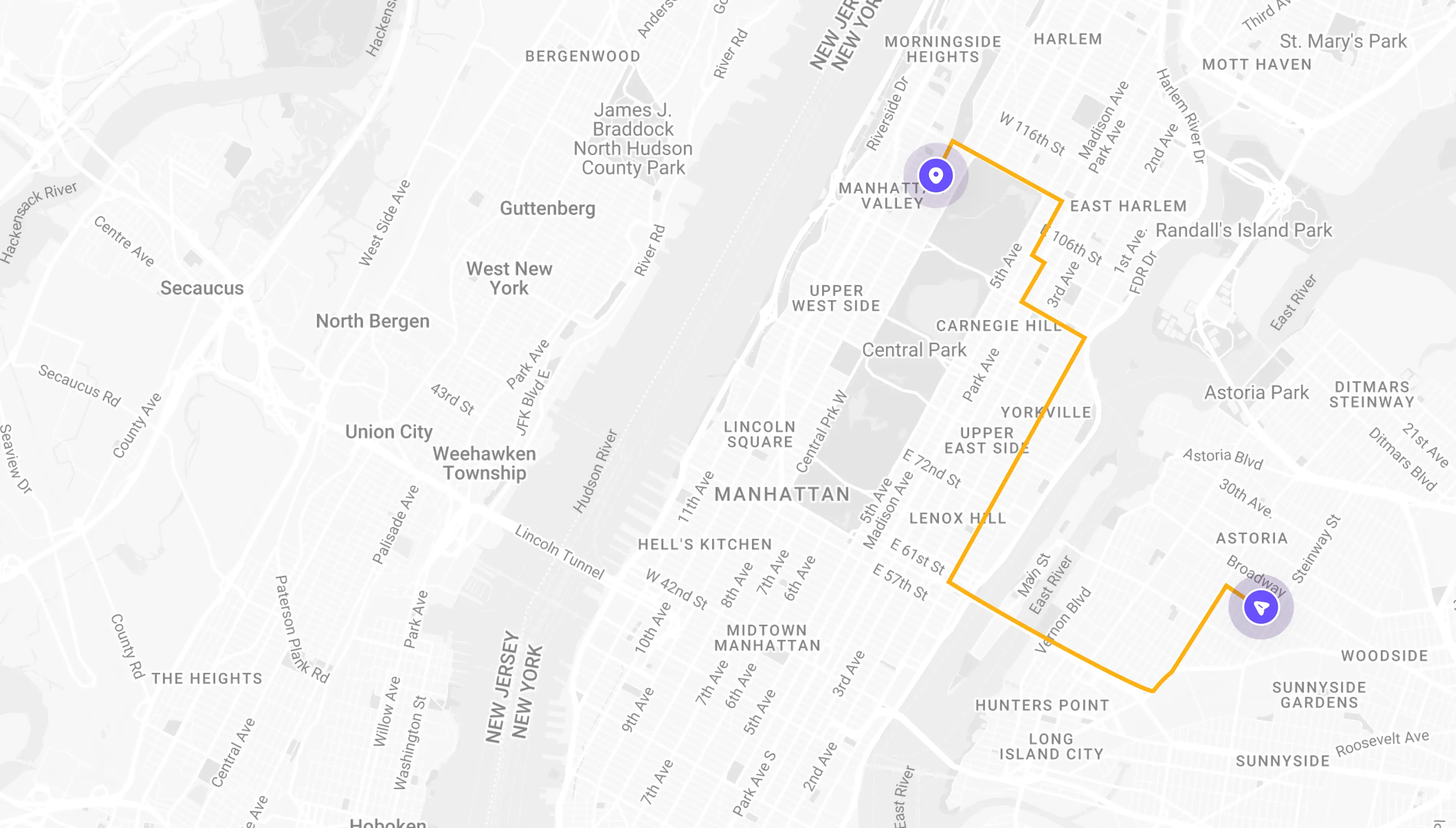
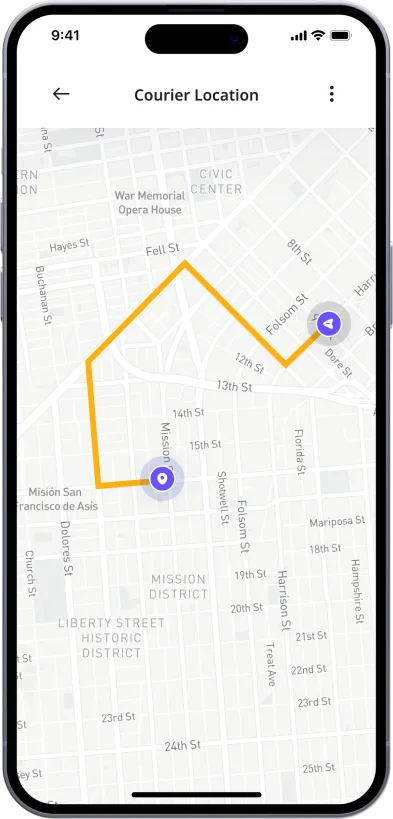
See If Delivery Is Available Near You
Delivery Not Available
Enter your ZIP code to check if prescription delivery is available in your area and how soon your meds could arrive.
How to get started
Choose your doctor, start a virtual visit, and have your prescriptions sent to your preferred pharmacy for pickup — all in just a few easy steps.
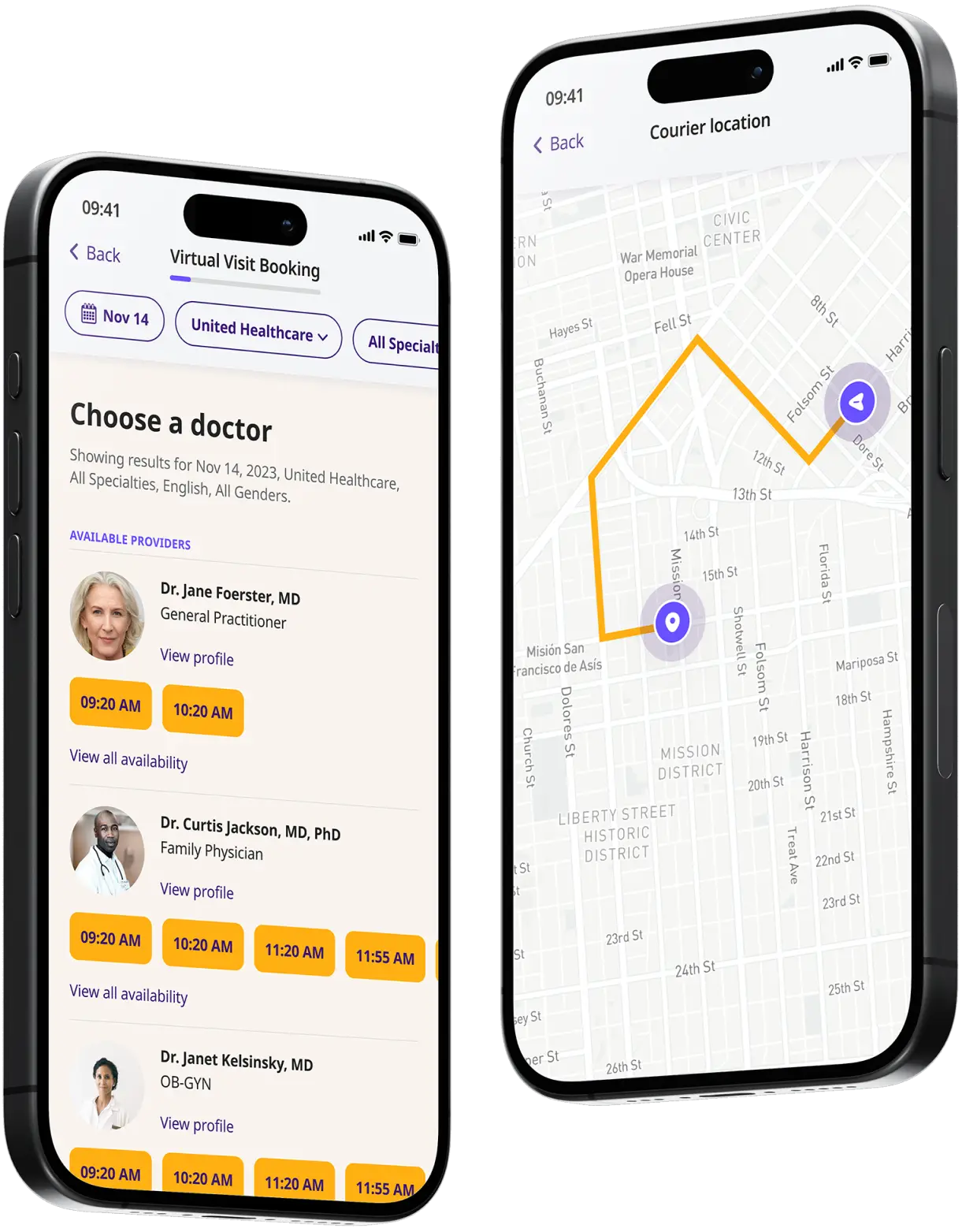
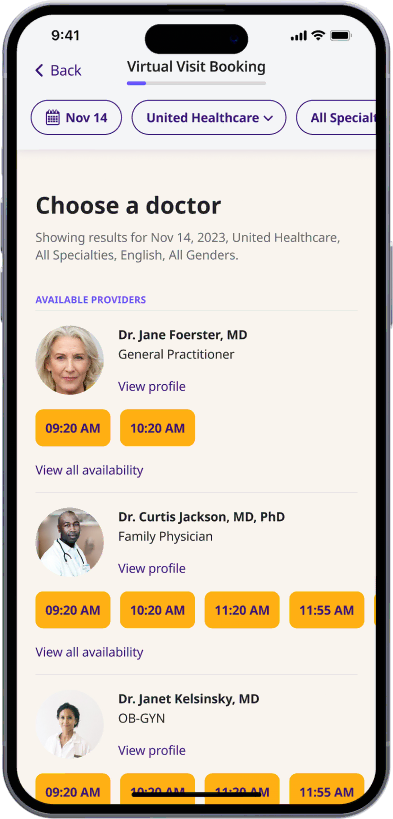
Choose a doctor
Choose a physician by availability, specialty, ratings, and more.
Start your video visit
Connect with a doctor in minutes on a secure video call.
Get your prescription
Pick up your meds or have them delivered in as little as an hour.
Available in 50 states. Insurance accepted.
One-Time
Physician Visit
One-time visit with a physician for diagnosis, treatment, Rx, labs, referrals, and doctor’s notes.
Accepted Insurances
See why people turn to DrHouse...
As seen in

Cellulitis Treatment Online
Cellulitis is a common, potentially serious bacterial skin infection that primarily affects the deeper layers of the skin and the fat and soft tissues underneath.
It is characterized by redness, swelling, warmth, and pain or tenderness in the affected area. If left untreated, cellulitis can rapidly spread, entering the lymph nodes and bloodstream, leading to life-threatening complications.
The skin normally hosts a variety of bacteria, but when there is a break in the skin barrier—such as cuts, abrasions, surgical incisions, or even minor scratches—these bacteria can enter and multiply, overwhelming the body’s ability to fight the infection.
The most common bacteria responsible for cellulitis are Streptococcus and Staphylococcus species, which are part of the natural flora of the skin but can cause problems when they penetrate the skin’s protective layers.
Cellulitis can occur on any part of the body but most frequently affects the skin on the lower legs. It is typically unilateral, meaning it usually occurs on just one side of the body. The skin appears swollen and red and may feel hot and tender to the touch.
The redness and swelling often spread rapidly. Individuals might also experience fever, chills, and swollen lymph nodes near the area of the infected skin.
The treatment of cellulitis primarily involves antibiotics to combat the infection. Early treatment is crucial to prevent the spread of the infection, which can lead to severe health problems, including sepsis, a life-threatening response to infection. Pain relief and measures to reduce swelling can also be part of treatment.
The condition has a high recurrence rate, and some individuals may experience repeated episodes of cellulitis, which requires additional medical attention.
Cellulitis symptoms
The symptoms of cellulitis can develop suddenly and progress rapidly, requiring prompt medical attention. Here are the key signs and symptoms to be aware of:
- Redness: The affected area of the skin usually appears red and may spread quickly. This redness often has well-defined borders that expand over a matter of hours or days.
- Swelling: Along with redness, the affected area typically swells. The swelling can make the skin feel tight and can sometimes limit movement if it occurs near a joint.
- Warmth: The skin over the affected area usually feels warm or hot to the touch, which is a clear indicator of inflammation and infection beneath the skin surface.
- Pain and tenderness: Cellulitis commonly causes pain or tenderness in the affected area. The intensity of the pain can vary, but it generally increases with pressure or when the area is touched.
- Fever: Many patients with cellulitis experience a fever, which may be accompanied by chills, sweating, or a general feeling of illness. The presence of fever suggests that the body is fighting off a significant infection.
- Blisters or skin lesions: In some cases, cellulitis can cause blisters or skin lesions to form on the infected skin. These may leak fluid and further complicate the skin’s condition.
- Red streaks: Red streaks leading from the affected area may develop. These streaks indicate that the infection may be spreading via the lymphatic system.
- Swollen lymph nodes: Nearby lymph nodes may swell in response to the infection, becoming tender to the touch. This is a sign that the body’s immune system is actively fighting the infection.
It is important for individuals to seek medical care if they notice these symptoms, especially if they occur suddenly and are associated with a fever or if the affected area is rapidly expanding.
Early medical intervention with appropriate antibiotic treatment can effectively manage cellulitis, prevent its spread, and avoid severe complications.
What causes cellulitis?
Cellulitis is primarily caused by an infection of the skin and underlying tissues with bacteria. The condition can arise from several factors that compromise the integrity of the skin barrier, allowing bacteria easy access to deeper tissue layers.
Here are the main causes and risk factors associated with cellulitis:
- Bacterial entry: The most common culprits for cellulitis are the bacteria Streptococcus and Staphylococcus. These bacteria can enter the skin through even very minor breaks in the skin, such as cuts, abrasions, burns, insect bites, surgical wounds, or sites of skin conditions like eczema or psoriasis.
- Skin Integrity: Individuals with conditions that damage the skin or cause chronic skin wounds, such as venous leg ulcers, diabetic ulcers, or fungal infections, are at increased risk of developing cellulitis.
- Underlying skin conditions: Eczema, athlete’s foot, and other dermatological conditions can cause cracks or breaches in the skin’s protective barrier, making it easier for bacteria to enter.
- Insect bites and animal bites: Bites from insects or animals not only break the skin but also can introduce bacteria directly into the tissues beneath the skin surface.
- Immune system function: Individuals with weakened immune systems, whether from conditions like diabetes, liver disease, kidney disease, or from the use of medications such as corticosteroids, are more susceptible to cellulitis. A weakened immune system may not fight off infections as effectively, allowing even ordinarily manageable bacterial invasions to escalate into serious infections.
- Circulatory issues: Poor circulation in the limbs, often a consequence of diabetes or peripheral artery disease, can contribute to skin ulcers and other disruptions of skin integrity. This not only makes it easier for bacteria to enter but also slows the healing process, increasing the risk of infection.
- Lymphedema: Swelling caused by excess fluid in body tissues can crack the skin and provide an entry point for bacteria. People with chronic lymphedema are at higher risk of recurrent cellulitis.
- Recent surgery or hospitalization: Surgical incisions provide a direct path for bacteria into the body’s internal tissues. Moreover, hospital-acquired infections can also lead to cellulitis if proper sterile techniques are not observed.
How to treat cellulitis?
Treatment strategies typically involve a combination of medication and self-care measures to manage symptoms and support recovery. Here’s an overview of the common approaches to treating cellulitis:
- Antibiotics: The cornerstone of cellulitis treatment is the use of antibiotics. These medications are prescribed to fight the bacterial infection. The type of antibiotic used depends on the severity of the infection and the suspected type of bacteria causing it. For mild cases of cellulitis, oral antibiotics such as penicillin, amoxicillin, or clindamycin may be prescribed for a course usually lasting 5 to 14 days. In more severe cases, or when symptoms are extensive or rapidly worsening, intravenous antibiotics may be required.
- Pain management: Over-the-counter pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) can help reduce fever and alleviate pain.
- Care of the affected area: Keeping the infected area elevated can help reduce swelling and relieve discomfort. It’s often recommended to elevate the affected limb higher than the heart to improve circulation and decrease swelling.
- Monitoring: Regular monitoring of the affected area is important to ensure that the infection is responding to treatment. If symptoms do not start to improve within a few days of starting antibiotics, or if they worsen, it’s crucial to contact a healthcare provider. This might mean the bacteria are resistant to the antibiotic, or there may be another underlying issue.
- Treating underlying conditions: If conditions such as edema, venous insufficiency, or a skin disorder are contributing to recurrent cellulitis, managing these underlying issues is vital to prevent future episodes. This may include using compression garments or treating the skin condition.
- Wound care: Proper care of any open wounds is essential, especially in diabetic patients or those with poor circulation. This includes regular cleaning and bandaging of affected areas to prevent bacteria from entering the skin.
Prompt and effective treatment of cellulitis is key to a full recovery and can prevent the progression to more serious health issues. In the context of telehealth, many aspects of cellulitis evaluation and management, particularly follow-up and monitoring during antibiotic treatment, can be handled remotely, ensuring that patients receive timely care without the need for in-person visits unless complications arise.
Cellulitis medication
The primary treatment for cellulitis involves antibiotic therapy, which is tailored to combat the specific bacteria suspected to be causing the infection.
The choice of medication and the duration of treatment depend on the severity of the infection, the patient’s overall health, and the presence of any underlying conditions. Here’s a detailed look at the typical medications used for treating cellulitis:
- Oral antibiotics: For most cases of mild to moderate cellulitis, oral antibiotics are prescribed. The choice of antibiotic is usually made based on the most likely bacteria causing the infection and the local antibiotic resistance patterns.
- Penicillin: Effective against many strains of Streptococcus, penicillin is often used for straightforward cases of cellulitis.
- Cephalexin (Keflex): A cephalosporin antibiotic, often used when patients are allergic to penicillin.
- Dicloxacillin: Effective against penicillinase-producing staphylococci, used primarily for cellulitis thought to be caused by staph bacteria.
- Clindamycin: Used in cases where patients are allergic to penicillin and cephalosporins, or when MRSA (Methicillin-resistant Staphylococcus aureus) is a suspected pathogen.
- Erythromycin and Azithromycin: Macrolide antibiotics, which are alternatives for those allergic to penicillin, though they may be less effective against some strains of bacteria.
- Pain relief medications: Pain associated with cellulitis can be intense. Over-the-counter pain relievers like acetaminophen or ibuprofen can help manage the discomfort and reduce fever.
- Topical antibiotics: While not typically used for treating the underlying infection in cellulitis, topical antibiotics may be used to treat or prevent superficial infections in cases where skin ulcers or wounds are also present.
- Adjunctive treatments: In cases where specific complications arise, additional medications might be needed. For example, if a patient develops an allergic reaction to an antibiotic, antihistamines might be prescribed.
Prevention of Cellulitis
Preventing cellulitis involves a combination of good hygiene practices, careful attention to skincare, and management of underlying health conditions that may increase the risk of infection. Here are key strategies for preventing cellulitis:
- Moisturize regularly: Keeping the skin moisturized prevents cracking and drying, which can lead to breaches in the skin’s protective barrier.
- Treat skin conditions: Conditions like eczema or athlete’s foot should be treated promptly to prevent them from causing cracks or tears in the skin.
- Use Protective Equipment: When engaging in activities that could injure the skin, such as gardening or sports, wear appropriate clothing and equipment to shield the skin from scrapes and cuts.
- Care for wounds: Clean all cuts, scratches, and abrasions immediately with soap and water. Apply a protective ointment and cover wounds with a sterile bandage to keep out bacteria.
- Hand washing: Regular hand washing is one of the most effective ways to prevent many types of infections, including those that can lead to cellulitis.
- Keep nails trimmed and clean: This helps prevent skin damage due to scratching and minimizes the risk of transferring bacteria from under the nails to the skin.
- Control blood sugar: For individuals with diabetes, maintaining control over blood sugar levels is crucial, as high sugar levels can weaken the immune system and slow healing.
- Improve circulation: Activities that improve blood flow, such as regular exercise, can help prevent complications from poor circulation, reducing the risk of skin infections.
- Be cautious in shared facilities: In places like gyms or pools, wear footwear to avoid fungal infections like athlete’s foot, which can lead to skin breaks.
- Animal and insect bites: Take precautions against insect bites and animal scratches, especially in environments where exposure is common.
- Early detection: Understanding the early signs of cellulitis (redness, swelling, pain, warmth, and fever) can lead to quicker treatment and prevent more serious infections.
- In severe cases: For individuals who experience recurrent cellulitis, especially in areas of lymphedema or past surgical sites, doctors may recommend low-dose antibiotics taken continuously as a preventive measure.
How DrHouse can help you with cellulitis
DrHouse is a telehealth service that provides comprehensive online care, making it an excellent resource for managing and treating conditions like cellulitis from the comfort of your home.
Here’s how DrHouse can assist patients in handling cellulitis effectively:
- Prompt online consultations: DrHouse offers quick access to healthcare professionals via video calls or chat, enabling patients to consult a doctor as soon as symptoms of cellulitis appear. Early diagnosis and treatment initiation are crucial for effective management and can prevent complications.
- Expert medical advice: DrHouse can connect patients with doctors who specialize in dermatology or infectious diseases, ensuring that you receive expert advice tailored to your specific health needs. Based on the severity of your cellulitis, doctors can provide personalized treatment plans that include prescription antibiotics, recommendations for over-the-counter pain relief, and guidance on wound care.
- Prescription services: The doctors at DrHouse can prescribe necessary medications, including oral antibiotics or topical ointments, and send the prescription directly to your preferred pharmacy for easy pickup. For patients with recurring cellulitis who need ongoing medication, DrHouse offers easy prescription refills without the need for repeated physical doctor visits.
- Follow-up care: Through follow-up video consultations, doctors can assess the healing process and make any necessary adjustments to your treatment plan. This continuous monitoring helps ensure that the cellulitis is responding to treatment and recovering properly.
- 24/7 availability: For urgent concerns or sudden worsening of symptoms, DrHouse offers 24/7 availability, giving patients peace of mind that help is always just a call or click away.
Using DrHouse for managing cellulitis not only simplifies the process of obtaining medical care but also enhances the quality of care through timely interventions and expert guidance.
This service transforms how patients approach and manage cellulitis, emphasizing convenience, effectiveness, and patient-centered care.
Frequently asked questions (FAQs)
Can cellulitis be diagnosed online?
Yes, with the help of telehealth services like DrHouse, cellulitis can be diagnosed through video consultations and assessments. Doctors can evaluate your symptoms and medical history, perform a visual examination of affected areas, and recommend appropriate treatment.
What is the most effective treatment for cellulitis?
The most effective treatment for cellulitis is a course of antibiotics prescribed by a doctor. Depending on the severity of the infection, other treatments may be recommended, such as pain relief medication or wound care measures.
Can cellulitis be treated with telehealth?
Yes, cellulitis can be effectively treated through telehealth services like DrHouse. Video consultations allow doctors to diagnose and monitor the condition, provide personalized treatment plans, and coordinate care with other healthcare providers if needed.
The online doctors at DrHouse can also prescribe antibiotics, making it a convenient option for managing cellulitis. However, in severe cases or if complications arise, in-person care may be necessary. In that case, DrHouse can assist with referrals and coordination for the best possible care.
Can I get medication for cellulitis online?
The doctors at DrHouse can prescribe antibiotics and other medications for cellulitis when appropriate. You can pick up the medication from your local pharmacy.
Related services
Explore more of our services tailored to your needs and discover additional ways we can support your healthcare needs.
Frequently asked questions