Eczema Treatment Online
Control eczema flare-ups with ease. See an online doctor for personalized treatment to soothe itching, dryness, and inflammation.
Available in 50 states. Insurance accepted.
Fast
virtual visits
24/7 care
assistants
Prescriptions
as needed

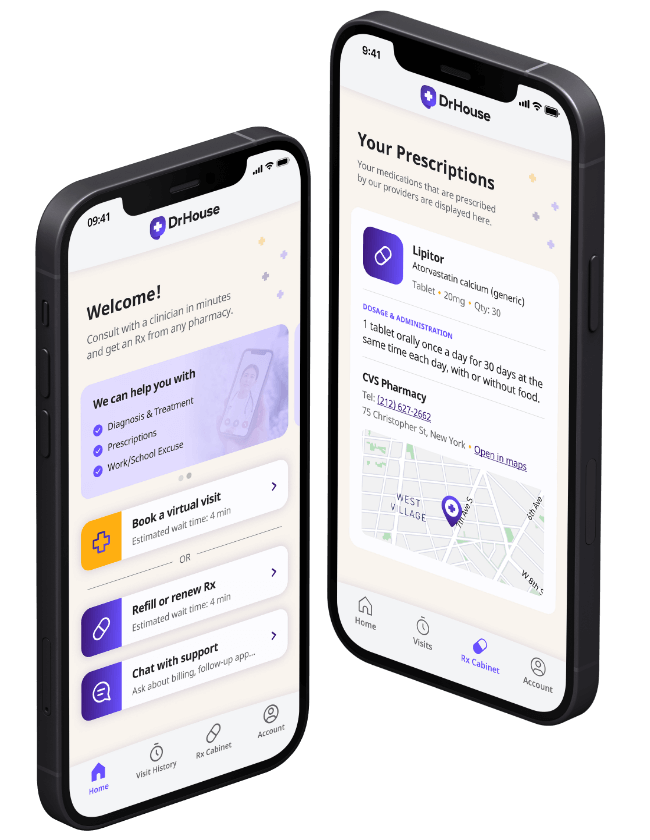
24/7 Personal Care
Consult with a physician in 15 minutes, refill an Rx or chat with our care assistants.

Affordable & Convenient
See your cost upfront and get treatment for hundreds of different conditions.

Insurance Accepted
We accept most major insurance plans, making healthcare easy and affordable.
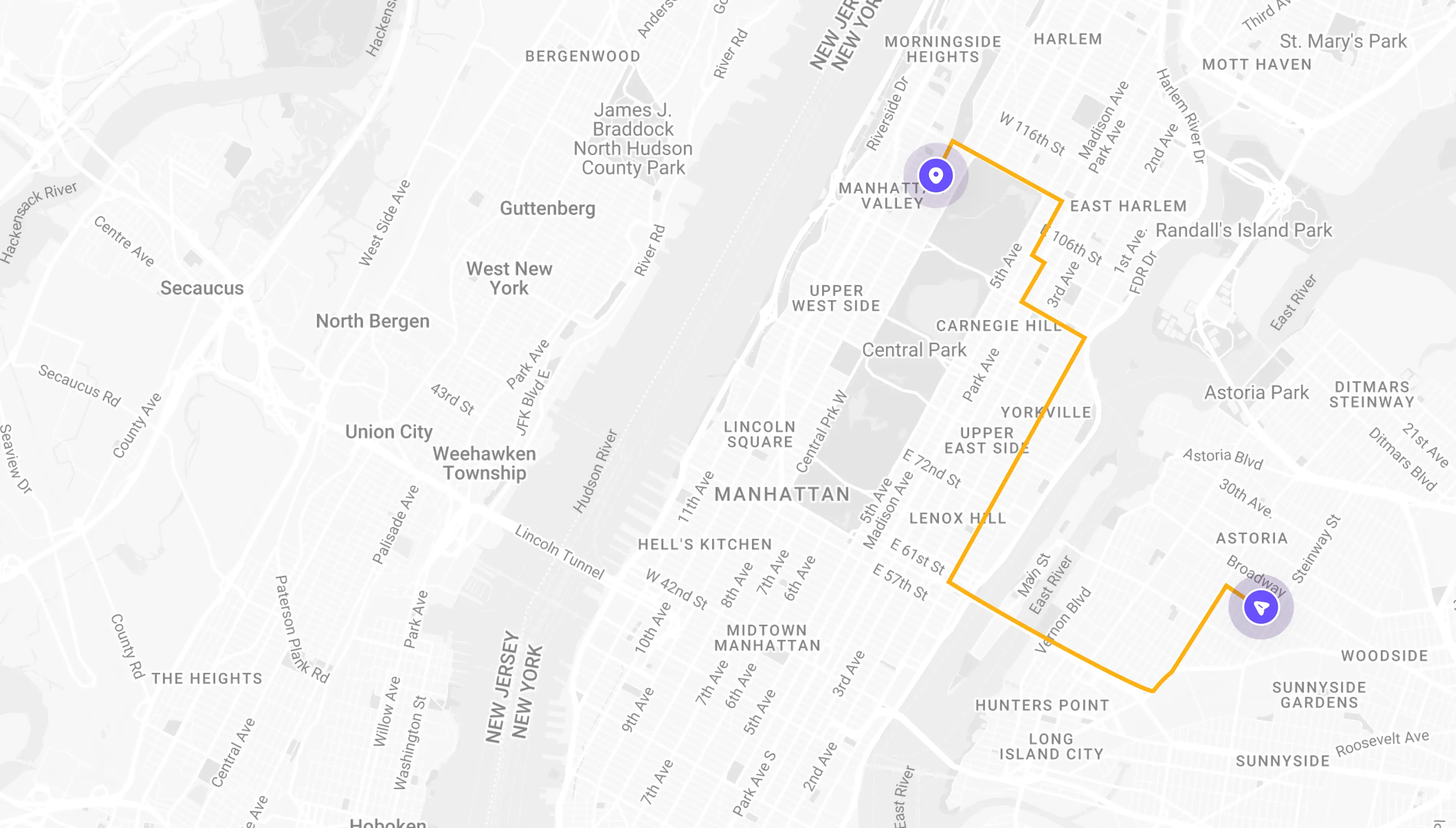
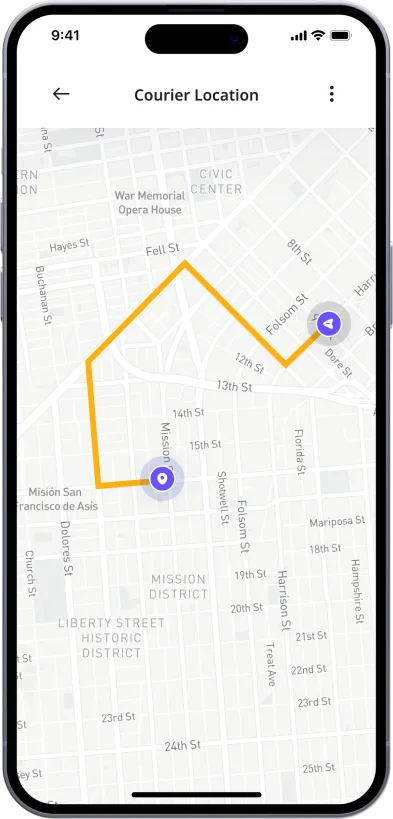
See If Delivery Is Available Near You
Delivery Not Available
Enter your ZIP code to check if prescription delivery is available in your area and how soon your meds could arrive.
How to get started
Choose your doctor, start a virtual visit, and have your prescriptions sent to your preferred pharmacy for pickup — all in just a few easy steps.
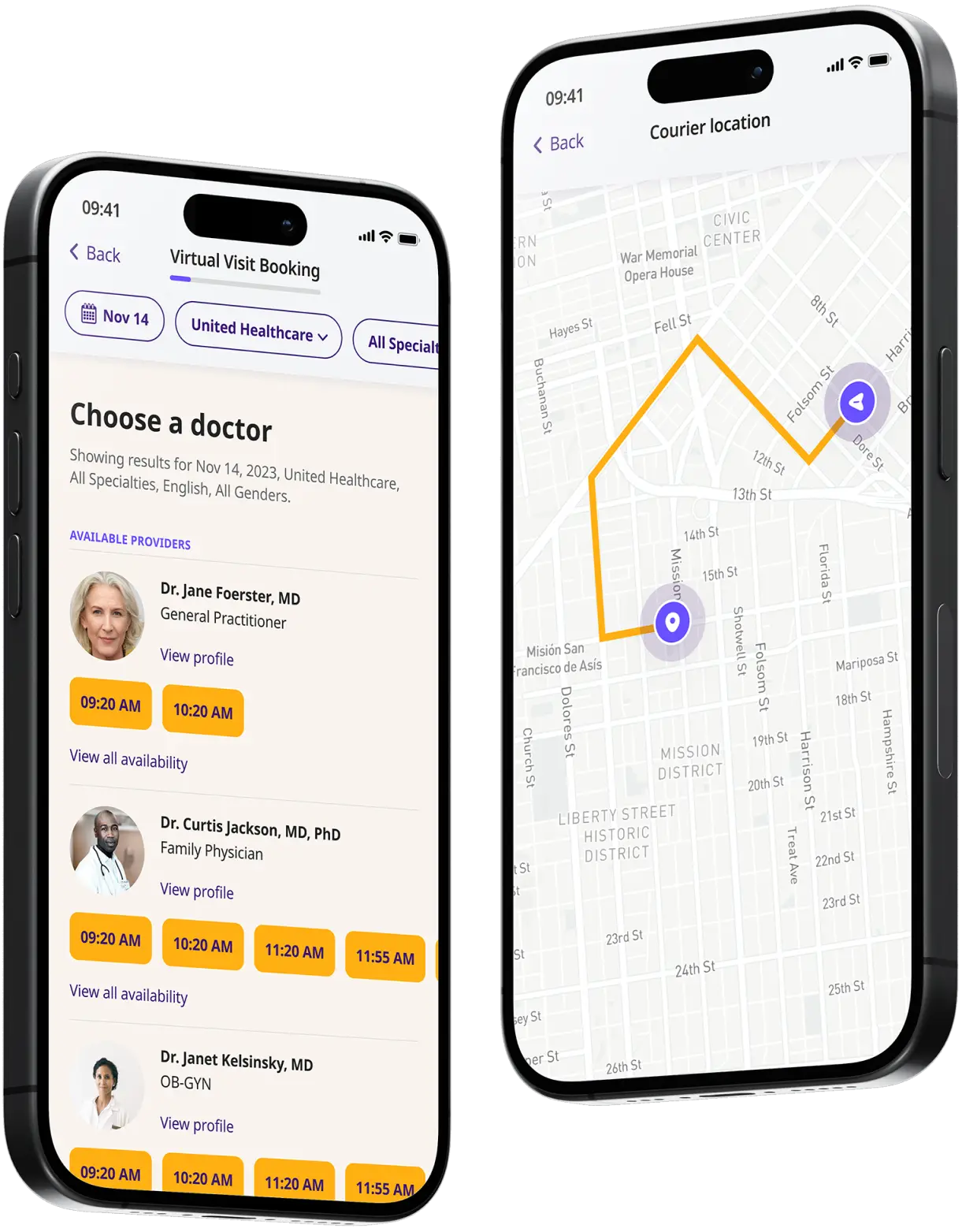
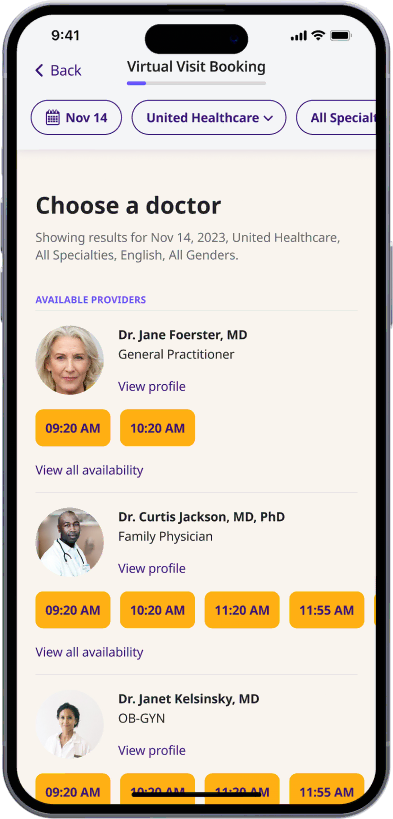
Choose a doctor
Choose a physician by availability, specialty, ratings, and more.
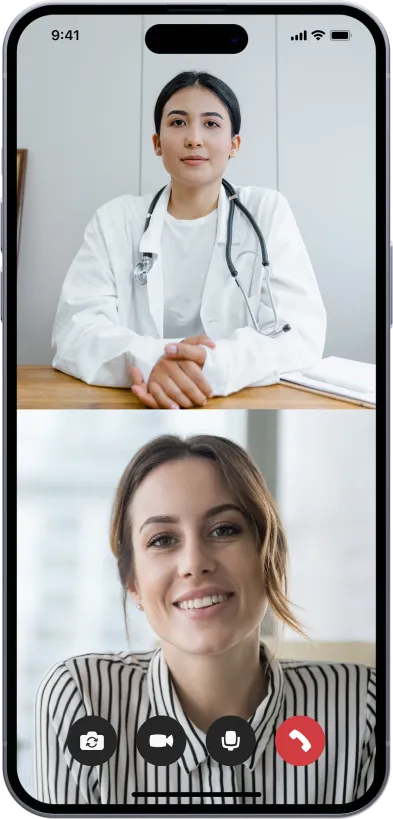
Start your video visit
Connect with a doctor in minutes on a secure video call.
Get your prescription
Pick up your meds or have them delivered in as little as an hour.
Available in 50 states. Insurance accepted.
One-Time
Physician Visit
One-time visit with a physician for diagnosis, treatment, Rx, labs, referrals, and doctor’s notes.
Accepted Insurances
See why people turn to DrHouse...
As seen in

Eczema Treatment Online
Eczema, also known as atopic dermatitis, is a chronic skin condition that affects millions of people worldwide. It is characterized by red, inflamed, itchy, and often cracked skin.
Although eczema can occur at any age, it is most commonly diagnosed in children and tends to flare periodically and then subside. The severity and symptoms of eczema can vary significantly from person to person.
This condition is not contagious, but its exact cause is not fully understood. Genetic factors play a key role, as eczema often runs in families. Environmental factors, such as allergens, irritants, and climate, also significantly impact the occurrence and severity of eczema flare-ups.
Living with eczema can be challenging due to the chronic itchiness and discomfort it causes, which can significantly affect sleep and daily activities. However, with proper management and treatment, most people can control their symptoms and lead healthy, comfortable lives.
Eczema symptoms
Eczema symptoms can vary widely but generally include the following key indicators:
- Itchiness: Often severe and can be more intense at night.
- Red to brownish-gray patches: Commonly appear on the hands, feet, ankles, wrists, neck, upper chest, eyelids, inside the bend of the elbows and knees, and in infants, the face and scalp.
- Small, raised bumps: These may leak fluid and crust over when scratched.
- Thickened, cracked, dry, scaly skin: These symptoms are especially noticeable during flare-ups.
- Raw, sensitive, swollen skin from scratching: Continuous scratching can further irritate the skin, leading to increased inflammation and risk of infection.
Eczema causes
Atopic dermatitis (Eczema) is a complex condition influenced by a combination of genetic, environmental, and immunological factors. Understanding these factors can help in managing the condition effectively.
- Genetic factors: Eczema often runs in families, suggesting a strong genetic component. People with eczema are likely to have a mutation in the gene responsible for creating filaggrin, a protein that contributes to maintaining a healthy, protective barrier on the top layer of the skin. This genetic defect can lead to a compromised skin barrier, making the skin more susceptible to irritation and infection.
- Environmental triggers: Eczema can be triggered or worsened by environmental factors. Common triggers include:
- Irritants: These can range from soaps and detergents to shampoos and disinfectants. Even rough fabrics like wool can irritate the skin.
- Allergens: Pollen, dust mites, pet dander, and molds are typical allergens that can trigger eczema.
- Microbes: Certain bacteria like Staphylococcus aureus, viruses, and certain fungi can cause flare-ups.
- Temperature and Humidity: Extremes of temperature and humidity can provoke eczema symptoms.
- Foods: Certain foods, particularly nuts, dairy, and soy products, can trigger symptoms in some people.
- Stress: Emotional stress is not a direct cause of eczema but can worsen the symptoms.
- Immune system dysfunction: Eczema is linked to an overactive immune system response. When people with eczema come into contact with an irritant or allergen, their immune system overreacts, leading to inflammation and eczema symptoms. This response is part of a complex interplay between immune cells and inflammatory signals in the skin.
- Skin barrier dysfunction: At the core of eczema is the dysfunction of the skin barrier. This barrier, when healthy, retains moisture and protects against bacteria, irritants, and allergens. In eczema, this barrier is weakened, which leads to moisture loss and vulnerability to infections.
- Hormonal changes: Hormonal changes, particularly those related to the menstrual cycle or pregnancy, can influence eczema symptoms.
Eczema treatment
Treating eczema effectively requires a multi-faceted approach, tailored to the individual’s symptoms and triggers. The goal of eczema treatment is to heal the affected skin and prevent flare-ups of symptoms.
Here’s an overview of the comprehensive treatment strategies:
- Moisturizing: Regularly applying moisturizers helps maintain skin hydration and repairs the skin barrier. This is fundamental in all eczema care regimens.
- Trigger avoidance: Identifying and avoiding triggers that worsen the eczema, such as certain soaps, foods, and allergens, is crucial.
- Topical treatments: These include corticosteroid creams and ointments that reduce inflammation and relieve itching. Topical calcineurin inhibitors, another class of drugs, help modulate immune responses directly in the skin.
- Medication: Over-the-counter remedies and prescription medications can control inflammation and treat infections. Antihistamines can also be used to reduce severe itching.
- Phototherapy: This involves exposing the skin to certain types of ultraviolet light. It’s particularly useful for severe eczema that doesn’t respond well to topical treatments.
- Lifestyle changes: Adjustments in diet, stress management, and daily habits can support treatment outcomes and reduce the frequency of flare-ups.
For severe cases, systemic medications that work throughout the body may be necessary. These include immunosuppressants that control the immune system’s overactivity related to eczema.
Eczema medication
Medications play a pivotal role in managing eczema, especially during flare-ups. The choice of medication often depends on the severity and location of the outbreak, as well as the patient’s age and overall health:
- Topical steroids: These are the most commonly prescribed medications for managing eczema and are effective in reducing skin inflammation and itchiness.
- Topical calcineurin inhibitors: Drugs like tacrolimus and pimecrolimus are useful as second-line treatments for managing moderate to severe eczema, particularly in sensitive areas where steroids are less desirable.
- Systemic medications: For extensive or severe eczema, systemic treatments such as cyclosporine, methotrexate, or mycophenolate mofetil may be used. These medications help suppress the immune system’s response.
- Biologics: Dupilumab is a relatively new class of biologic medication approved for treating moderate to severe eczema. It targets a specific part of the immune system known to play a key role in inflammatory processes.
- Antibiotics: If eczema is complicated by a skin infection, antibiotics may be prescribed to clear the infection.
- Antihistamines: These can help reduce itching, particularly at night, to aid better sleep.
Each medication has specific uses, benefits, and potential side effects, and they are usually part of a broader treatment plan that includes skincare routines and lifestyle adjustments.
Treating and diagnosing eczema online
Treating and diagnosing eczema online through telehealth services like DrHouse is both feasible and effective. The process typically involves the following steps:
- Consultation: Patients schedule an online appointment and consult with a healthcare provider via video, chat, or phone. During this session, patients can discuss their symptoms and medical history.
- Diagnosis: Although a physical exam is ideal, doctors can often diagnose eczema based on the patient’s history and a detailed description of symptoms. In some cases, patients may be asked to provide photos of the affected areas.
- Treatment plan: Based on the diagnosis, the healthcare provider can prescribe medications, recommend over-the-counter solutions, and suggest lifestyle adjustments to manage the symptoms. Prescriptions can be sent directly to a local pharmacy.
- Follow-up: Telehealth platforms typically offer follow-up appointments to assess the effectiveness of the treatment and make any necessary adjustments.
This approach allows patients to receive timely eczema management advice and prescriptions without the need to visit a clinic in person.
Frequently asked questions (FAQs)
Can online doctors treat eczema?
Yes, DrHouse can effectively treat eczema through its telehealth services. Online doctors are equipped to diagnose and manage eczema by conducting virtual consultations where they review symptoms, medical history, and sometimes photos of affected areas.
Following a comprehensive evaluation, the online doctor can prescribe medications, provide over-the-counter recommendations, and suggest lifestyle changes to help control eczema symptoms.
Can I get an online prescription for eczema medication from DrHouse?
Yes, you can receive an online prescription for eczema medication from DrHouse. After a thorough virtual consultation, the healthcare provider can determine the most suitable treatment plan and prescribe necessary medications. This prescription will then be sent directly to your preferred local pharmacy, allowing you to begin managing your eczema without the need for an in-person clinic visit.
Related services
Explore more of our services tailored to your needs and discover additional ways we can support your healthcare needs.
Frequently asked questions