Rash Treatment Online
Ease rash symptoms like redness and itching fast. DrHouse offers expert online treatment and 24/7 doctor access.
Available in 50 states. Insurance accepted.
Fast
virtual visits
24/7 care
assistants
Prescriptions
as needed



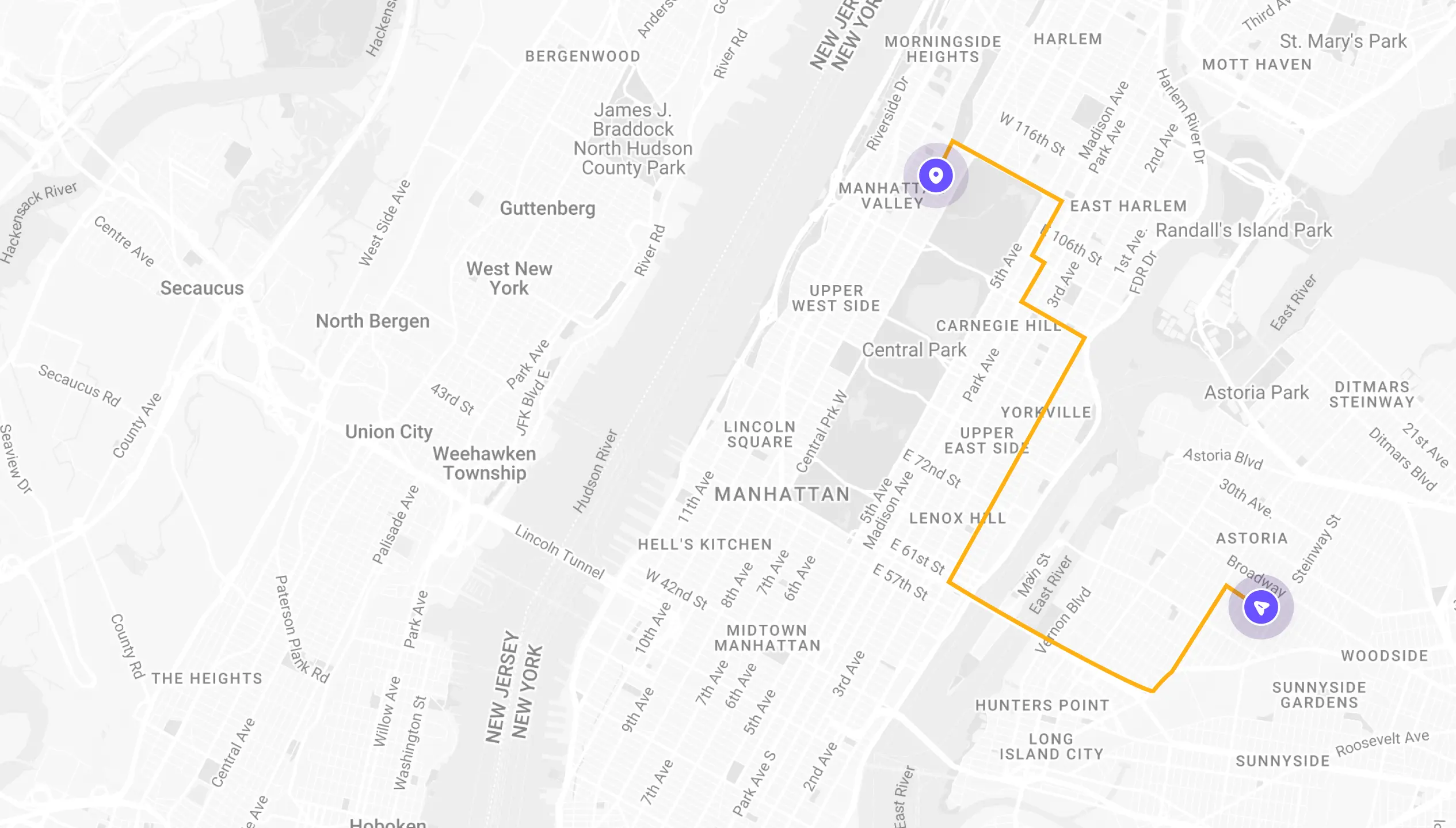
See If Delivery Is Available Near You
Delivery Not Available
Enter your ZIP code to check if prescription delivery is available in your area and how soon your meds could arrive.
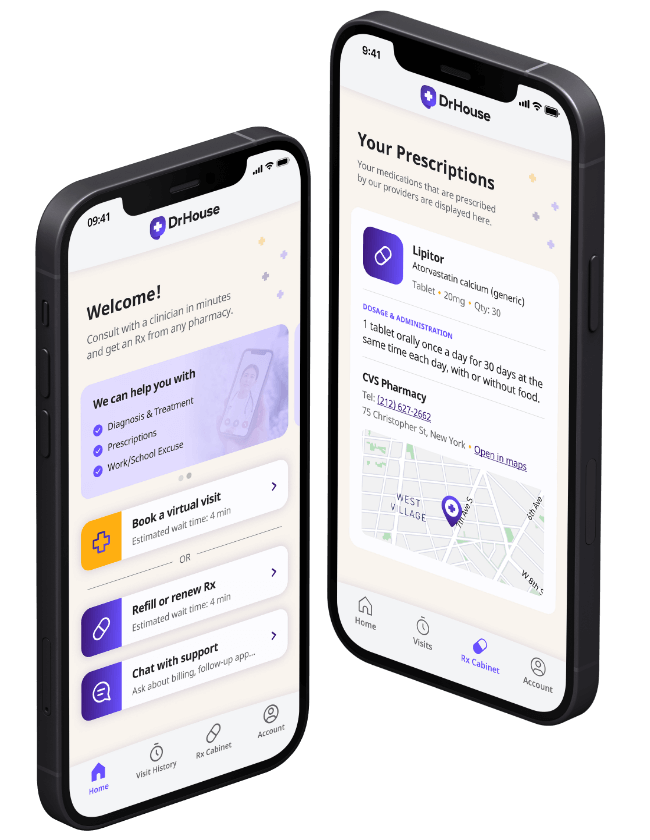
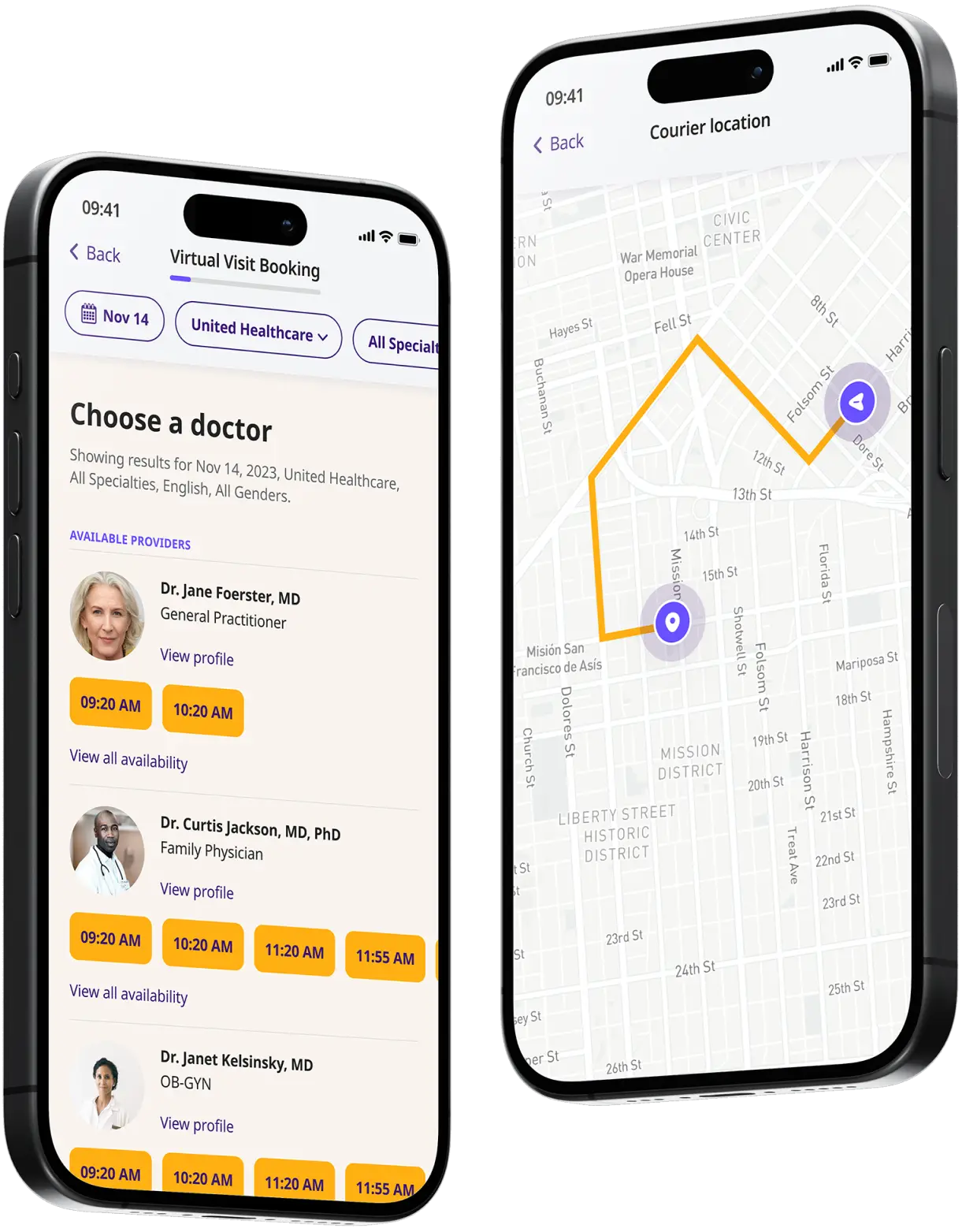
How to get started
Choose your doctor, start a virtual visit, and have your prescriptions sent to your preferred pharmacy for pickup — all in just a few easy steps.
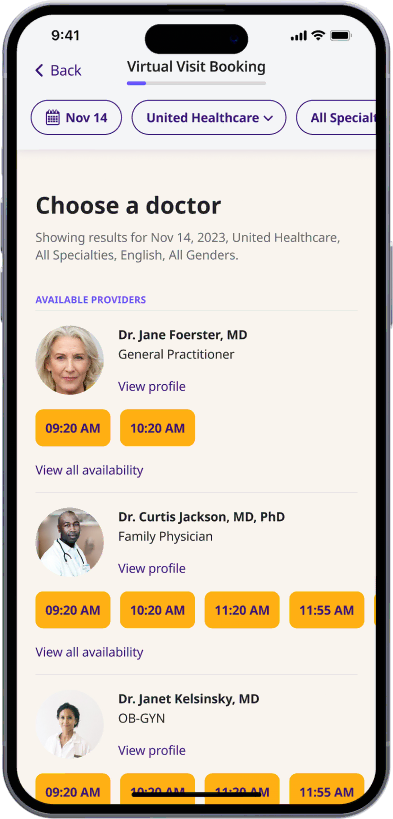
Choose a doctor
Choose a physician by availability, specialty, ratings, and more.
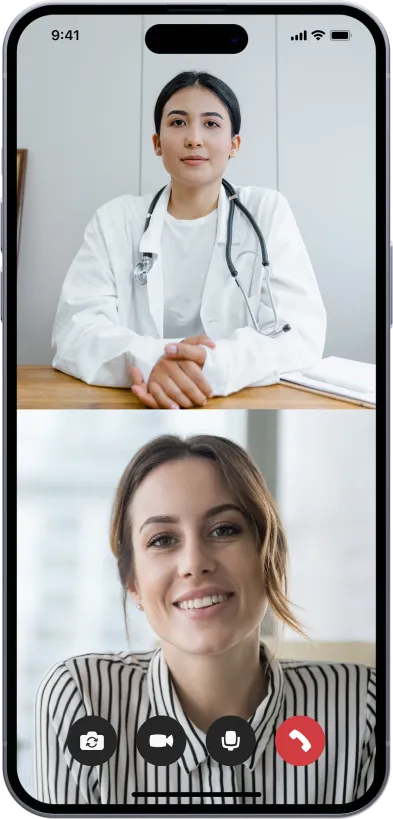
Start a video call
Get connected with a doctor anytime, anywhere.
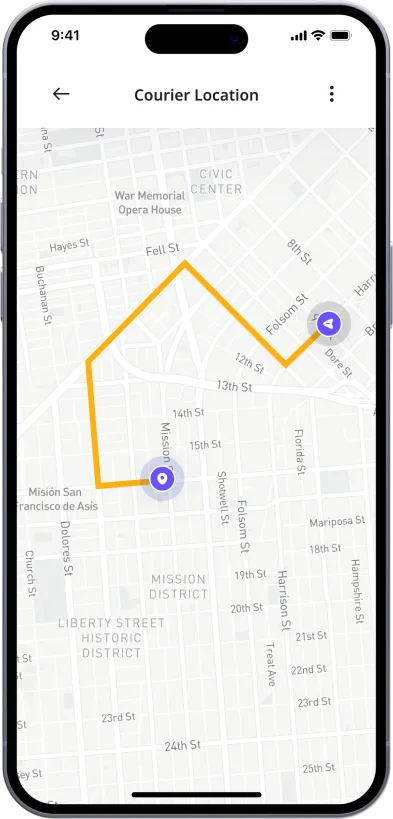
1-Hour Rx Delivery
Your prescription delivered to your door in 1 hour or less.
Available in 50 states. Insurance accepted.
One-Time
Physician Visit
One-time visit with a physician for diagnosis, treatment, Rx, labs, referrals, and doctor’s notes.
Accepted Insurances
See why people turn to DrHouse...
As seen in

Rash Treatment Online
Common causes for rashes
Rashes are a common dermatological condition that can arise due to various causes, ranging from infections and allergies to chronic diseases. Here are some common causes for rashes:
- Allergic reactions: Allergic reactions are a primary cause of rashes, often manifesting as hives or eczema. These reactions can be triggered by food, medications, insect stings, or contact with allergenic substances like latex or nickel. Common symptoms include itchy skin, red patches, and swelling.
- Infections: Both bacterial and viral infections can lead to rashes. For example, impetigo, caused by staphylococcus or streptococcus bacteria, results in red sores that quickly rupture and ooze. Viral infections such as measles or chickenpox are marked by distinctive red, spotty rashes across the body.
- Autoimmune disorders: Autoimmune disorders like lupus or psoriasis trigger the body’s immune system to attack healthy cells, leading to inflammation and rash. Psoriasis typically causes scaly, itchy patches of skin, while lupus might cause a butterfly-shaped rash on the face.
- Heat and sweat: Heat rash, or miliaria, occurs when sweat ducts get blocked during hot, humid weather. This condition is characterized by small, itchy bumps or blisters, especially in clothed areas of the body, which are prone to sweating.
- Contact dermatitis: This is a localized rash that occurs when the skin comes into contact with an irritant or allergen. Common irritants include laundry detergents, soaps, cosmetics, and plants like poison ivy. The skin may appear red, itchy, and inflamed after exposure.
- Medications: Certain medications can cause adverse skin reactions, including rashes. Antibiotics, anti-seizure drugs, and diuretics are known to trigger allergic skin reactions in some individuals. These rashes can range from mild to severe and may require immediate medical attention.
- Chronic skin conditions: Conditions like eczema (atopic dermatitis) and rosacea persistently affect the skin, causing redness, irritation, and sometimes peeling. These conditions often require long-term management strategies and can flare up sporadically.
- Environmental factors: Exposure to certain chemicals, plants, and even extreme weather conditions can induce rashes. For instance, cold weather can dry out the skin, leading to redness and itching, while exposure to industrial chemicals might cause a chemical burn or dermatitis.
- Insect bites and parasitic infestations: Insect bites from mosquitoes, fleas, and bedbugs can cause localized itching and rashes. Parasitic infestations like scabies, caused by mites burrowing into the skin, result in intense itching and a pimple-like rash.
- Underlying health conditions: Sometimes, a rash is a symptom of an underlying health issue, such as kidney disease or liver disease, which can cause itching and changes in skin color.
How are skin rashes treated?
Treating skin rashes effectively involves several strategies tailored to the underlying cause and severity of the rash. Here are some common treatments:
- Topical medications: Creams and ointments containing corticosteroids are frequently prescribed to reduce inflammation and itching. Antifungal creams are used for rashes caused by yeast or fungus, and antibiotic creams address bacterial infections.
- Oral medications: For severe cases, oral medications like antihistamines can help relieve itching, and oral corticosteroids might be used to control severe inflammation. In cases of infection, oral antibiotics or antivirals are necessary.
- Lifestyle changes and home remedies: Simple home care practices can alleviate symptoms. These include using mild soaps, applying cool, wet compresses to irritated areas, and wearing loose, soft clothing to avoid irritation.
- Avoidance of irritants: Identifying and avoiding irritants or allergens is critical. This may involve changing detergents, and soaps, or avoiding certain foods or medications known to cause allergic reactions.
- Light therapy: For chronic conditions like psoriasis, phototherapy involving controlled exposure to ultraviolet light can be beneficial.
- Specialized treatments: Treatments like immunomodulators are used for chronic inflammatory conditions like eczema, targeting the immune system to reduce flare-ups.
Medication for skin rashes
Effective treatment of skin rashes often involves medication tailored to the specific type and cause of the rash. Here are several commonly prescribed medications:
- Topical corticosteroids: These creams and ointments reduce inflammation and are used for a variety of rashes, such as eczema and dermatitis.
- Antihistamines: Oral antihistamines can relieve itching and swelling associated with allergic rashes.
- Antimicrobial treatments: Antifungal creams are used for fungal infections, while antibiotic creams or oral antibiotics are prescribed for bacterial infections.
- Immunosuppressants: For severe or chronic conditions like psoriasis, medications that modify the immune response, such as cyclosporine, can be effective.
- Biologics: Targeted biologic therapies are used for conditions like severe psoriasis, targeting specific parts of the immune system.
- Over-the-counter options: Mild rashes often respond well to over-the-counter hydrocortisone creams and moisturizers.
How can DrHouse help?
DrHouse offers a comprehensive telehealth service that simplifies access to healthcare for skin rash treatment. Here’s how DrHouse can assist:
- Diagnosis and treatment: Our board-certified doctors can diagnose the cause of your rash and develop a personalized treatment plan online.
- Prescription medications: Our doctors can prescribe topical or oral medications as necessary for your specific condition.
- Follow-up care: DrHouse offers follow-up appointments to ensure that your skin rash is improving and adjust treatment if needed.
- 24/7 access: Our telehealth service is available 24/7, so you can receive care anytime, anywhere.
- Convenience and privacy: With DrHouse, you can receive treatment from the comfort of your own home without having to schedule an in-person appointment. This also allows for greater privacy for sensitive skin conditions.
Frequently asked questions (FAQs)
Can skin rashes be treated online?
Yes, skin rashes can be treated through online telehealth services like DrHouse. Our board-certified doctors can diagnose and treat a variety of skin rashes through virtual appointments.
Do I need to provide photos of my rash for an online appointment?
Providing photos of your rash is highly recommended for accurate diagnosis and treatment. You can easily upload photos during your virtual appointment with DrHouse.
Can I get prescription medication for a rash online from DrHouse?
Yes if our doctors determine that medication is necessary for your rash, they can prescribe topical or oral medication during your virtual appointment.
Related services
Explore more of our services tailored to your needs and discover additional ways we can support your healthcare needs.
Frequently asked questions