Get a Prescription for Antifungals Online
Treat fungal infections quickly with online antifungal prescriptions from the physicians at DrHouse. Available 24/7!
Available in 50 states. Insurance accepted.
Fast
virtual visits
24/7 care
assistants
Prescriptions
as needed

24/7 Personal Care
Consult with a physician in 15 minutes, refill an Rx or chat with our care assistants.

Affordable & Convenient
See your cost upfront and get treatment for hundreds of different conditions.

Insurance Accepted
We accept most major insurance plans, making healthcare easy and affordable.
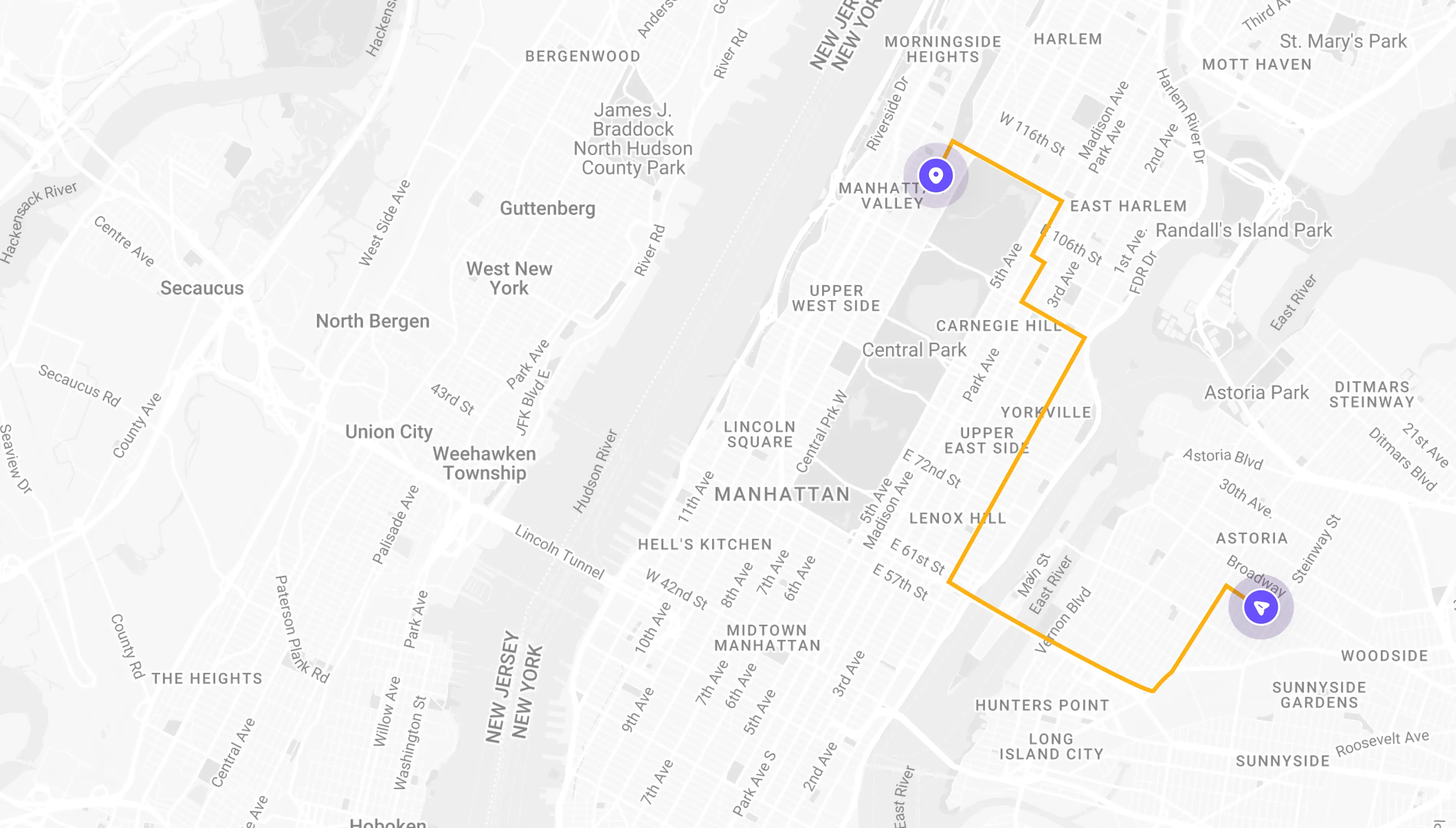
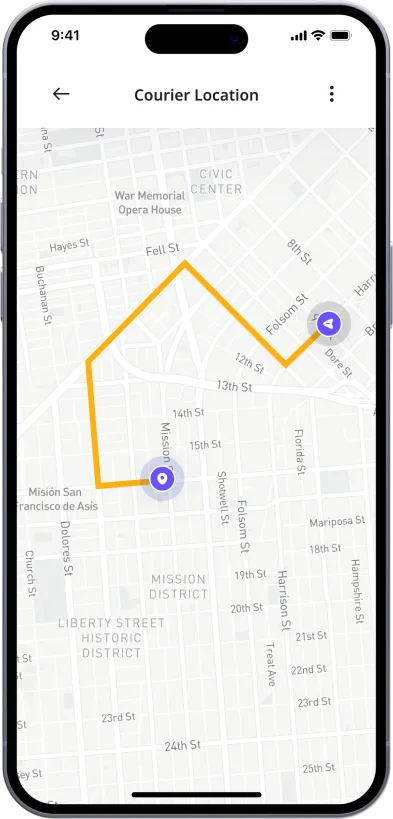
See If Delivery Is Available Near You
Delivery Not Available
Enter your ZIP code to check if prescription delivery is available in your area and how soon your meds could arrive.
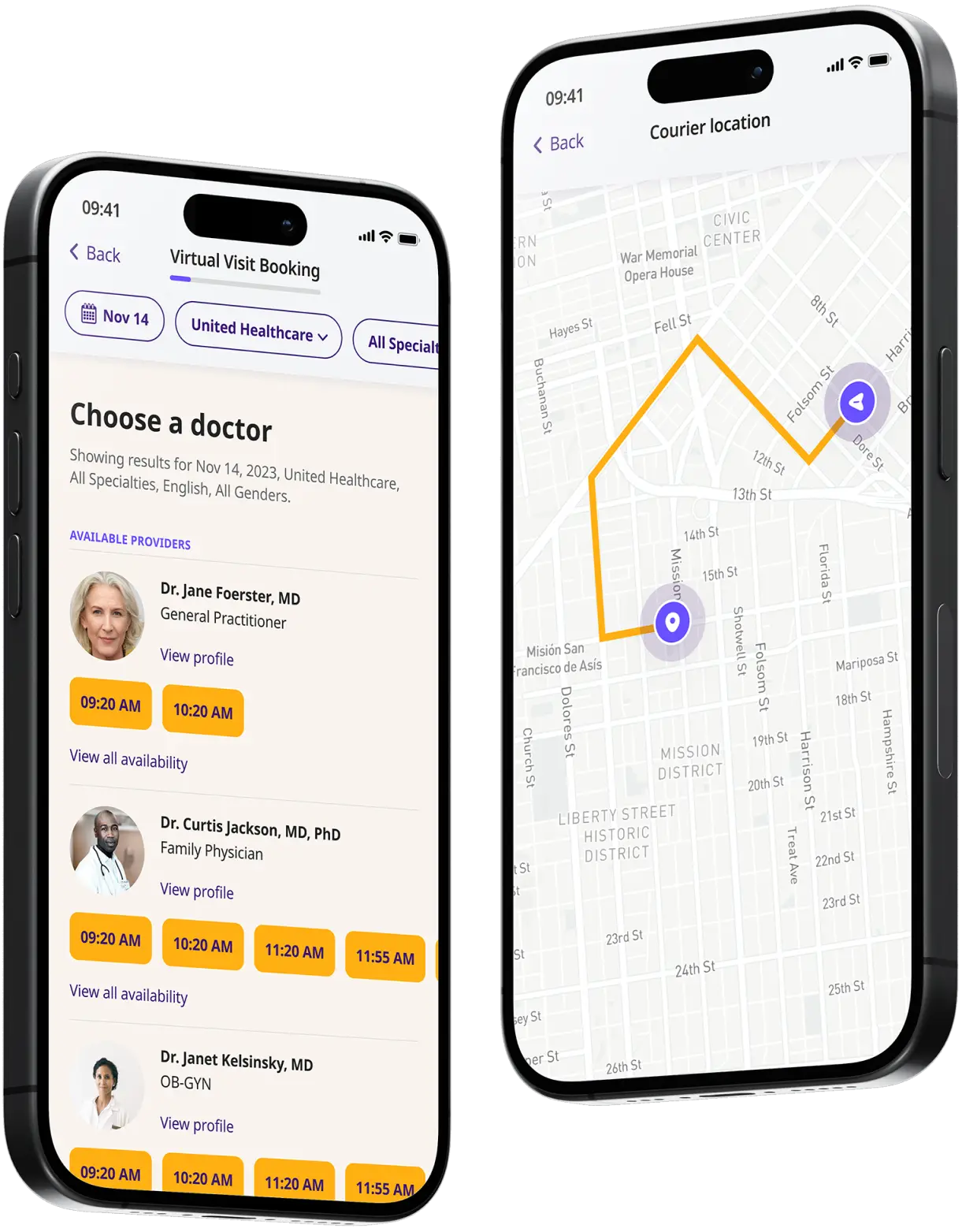
How to get started
Choose your doctor, start a virtual visit, and have your prescriptions sent to your preferred pharmacy for pickup — all in just a few easy steps.
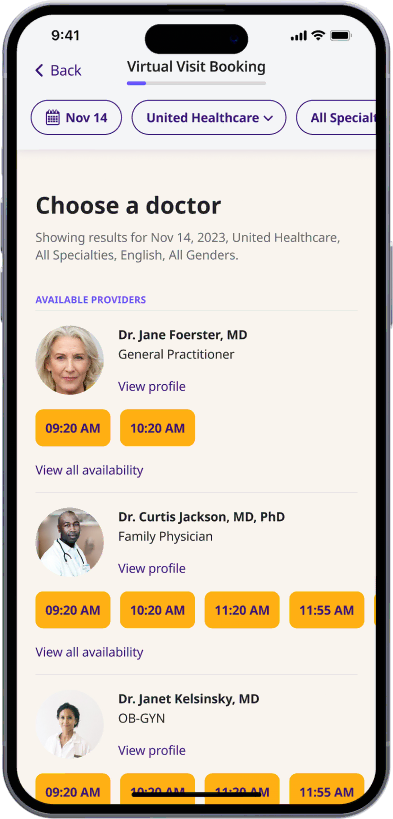
Choose a doctor
Choose a physician by availability, specialty, ratings, and more.
Start your video visit
Connect with a doctor in minutes on a secure video call.
Get your prescription
Pick up your meds or have them delivered in as little as an hour.
Available in 50 states. Insurance accepted.
One-Time
Physician Visit
One-time visit with a physician for diagnosis, treatment, Rx, labs, referrals, and doctor’s notes.
Accepted Insurances
See why people turn to DrHouse...
As seen in

Antifungal Medication
What are antifungals?
Antifungals are a class of medications designed to treat fungal infections, which can affect various parts of the body including the skin, nails, and internal organs.
These medications are crucial for combating pathogens that cause conditions ranging from superficial infections, like athlete’s foot and ringworm, to more severe systemic infections such as candidiasis or cryptococcal meningitis.
Antifungals work by targeting the cellular structure of fungi to either halt their growth or kill them directly. This treatment approach is essential because fungal cells are eukaryotic and share many similarities with human cells, making selective targeting a critical factor in treatment efficacy and safety.
Given the broad spectrum of fungal infections, antifungal medications come in various forms, including creams, ointments, pills, and injections, to address specific needs and infection sites.
Common conditions that are treated with antifungals
Antifungal medications are used to treat a wide range of fungal infections, which can affect different parts of the body. Here are some of the most common conditions that are effectively managed with antifungal treatments:
- Athlete’s foot (tinea pedis) – A fungal infection that typically begins between the toes and can spread to other parts of the foot.
- Ringworm (tinea corporis) – Not caused by a worm, but by a fungus affecting the skin, typically appearing as a round, red, itchy rash.
- Jock itch (tinea cruris) – A fungal infection of the groin and thighs, common in athletes and people who sweat a lot.
- Yeast infections (candidiasis) – Overgrowth of Candida yeast can affect the mouth (thrush), throat, skin, and genitals, including vaginal yeast infections.
- Onychomycosis (fungal nail infections) – Infection that results in discolored, thickened, and often brittle nails.
- Scalp ringworm (tinea capitis) – A fungal infection of the scalp, primarily affecting children, characterized by hair loss and scaly patches.
- Fungal meningitis – A rare condition that involves swelling of the protective membranes covering the brain and spinal cord, usually caused by the spread of a fungus through blood to the spinal cord.
- Aspergillosis – An infection caused by Aspergillus, a common mold that lives indoors and outdoors. This infection mainly affects people with weakened immune systems or lung diseases.
- Cryptococcal meningitis – A serious fungal infection of the brain that primarily affects people with compromised immune systems, such as those with HIV/AIDS.
- Pneumocystis pneumonia (PCP) – A fungal infection that affects the lungs, commonly seen in people with weakened immune systems, such as those undergoing chemotherapy or with HIV/AIDS.
- Histoplasmosis – An infection caused by breathing in spores of a fungus often found in bird and bat droppings. It primarily affects the lungs but can also spread throughout the body.
- Coccidioidomycosis (valley fever) – An infection caused by inhaling the spores of Coccidioides fungus, found in the soil of specific regions, primarily the southwestern United States.
Types of antifungal medication
Antifungal medications are classified based on their chemical structure and the mechanism through which they combat fungal infections. Understanding the different types ensures that the most effective medication is chosen for a particular type of fungal infection. Here are the primary types of antifungal medications:
- Azoles: Imidazoles and Triazoles are the two main groups in this category. These medications inhibit the synthesis of ergosterol, a key component of the fungal cell membrane, leading to increased membrane permeability and cell death. Commonly used azoles include fluconazole, itraconazole, and ketoconazole. They are used to treat a wide range of infections, from superficial skin infections to more serious systemic infections.
- Polyenes: These drugs bind to ergosterol and create pores in the fungal cell membrane, causing cell components to leak out and leading to cell death. Amphotericin B and nystatin are polyenes, often used in severe fungal infections or as a topical treatment, respectively.
- Echinocandins These are a newer class of antifungal drugs that inhibit the synthesis of β-glucan, an essential component of the fungal cell wall. By disrupting the cell wall, echinocandins contribute to cell lysis and death. Drugs in this class, such as caspofungin, micafungin, and anidulafungin, are typically used to treat invasive candidiasis and other serious fungal infections.
- Allylamines: Allylamines inhibit the enzyme squalene epoxidase, which is involved in ergosterol synthesis. By halting this process, they cause the accumulation of toxic intermediates and disrupt cell membrane function. Terbinafine is a well-known allylamine used primarily for treating fungal infections of the skin and nails.
- Thiocarbamates: Similar to allylamines, thiocarbamates inhibit squalene epoxidase. Tolnaftate, a common thiocarbamate, is used primarily in the treatment of athlete’s foot and other tinea infections.
- Morpholines: These antifungals inhibit enzymes involved in ergosterol synthesis, leading to a depletion of ergosterol and an accumulation of toxic intermediates in the fungal cell membrane. Amorolfine is used to treat skin and nail infections.
Each type of antifungal medication has specific indications, advantages, and limitations. The choice of medication often depends on the type of fungal infection, the location of the infection, the patient’s health status, and potential interactions with other medications.
How does antifungal medication work?
Antifungal medications combat fungal infections by targeting the biological processes essential for the survival and growth of fungal cells. The effectiveness of these medications hinges on their ability to exploit differences between human cells and fungal cells, minimizing harm to the human host while effectively eradicating the infection.
Here are the primary mechanisms by which antifungal medications operate:
- Targeting the cell membrane: Most antifungals, such as azoles and polyenes, focus on disrupting the synthesis or function of ergosterol, a vital component of the fungal cell membrane. Azoles inhibit an enzyme (lanosterol 14α-demethylase) needed for ergosterol production, leading to increased membrane permeability and eventually cell death. Polyenes, such as amphotericin B, bind directly to ergosterol, creating pores that cause crucial cell contents to leak out, which is fatal to the fungal cell.
- Interfering with cell wall synthesis: Echinocandins like caspofungin, micafungin, and anidulafungin inhibit the synthesis of β-glucan, an essential component of the fungal cell wall. This inhibition weakens the structural integrity of the cell wall, causing the cell to become unstable and unable to withstand osmotic pressure, leading to cell lysis.
- Blocking nucleic acid synthesis: Some antifungals can interfere with the synthesis of DNA and RNA within the fungal cell, hindering its ability to replicate and proliferate. Flucytosine, for example, is converted into a compound that disrupts DNA synthesis and protein synthesis, effectively halting fungal growth.
- Inhibiting microtubule function: Griseofulvin works by binding to microtubules, preventing them from forming the mitotic spindle necessary for cell division. This action specifically hampers the division of fungal cells, slowing the spread of the infection.
Each class of antifungal medications is selectively effective against certain types of fungi, which is why the specific pathogen causing the infection must be identified to choose the most effective treatment. This targeted approach helps reduce the fungal population while aiming to preserve human cells and minimize potential side effects.
Side effects of antifungal medication
Antifungal medications can also cause a range of side effects. These side effects vary depending on the type of antifungal drug, the duration of treatment, and the individual patient’s response. Here are some common side effects associated with different types of antifungal medications:
Azoles (e.g., Fluconazole, Itraconazole, Ketoconazole):
- Gastrointestinal issues: Nausea, vomiting, abdominal pain, and diarrhea.
- Liver toxicity: Elevated liver enzymes, hepatitis, and in rare cases, severe liver injury.
- Endocrine effects: Hormonal imbalance, including changes in testosterone and cortisol levels, particularly with ketoconazole.
- Skin reactions: Rash and, in rare cases, more severe reactions such as Stevens-Johnson syndrome.
Polyenes (e.g., Amphotericin B, Nystatin):
- Infusion reactions: Fever, chills, headache, and shaking, often occurring shortly after administration of amphotericin B.
- Kidney damage: Amphotericin B can cause renal impairment, which may be reversible upon completion of treatment but requires careful monitoring.
- Electrolyte imbalances: Issues such as hypokalemia (low potassium) and hypomagnesemia (low magnesium), which can affect heart and muscle function.
Echinocandins (e.g., Caspofungin, Micafungin, Anidulafungin):
- Infusion-related reactions: Including rash, itching, facial swelling, and anaphylaxis in severe cases.
- Hepatic effects: Mild liver enzyme elevations and rarely, more severe hepatic dysfunction.
- Gastrointestinal symptoms: Nausea and diarrhea are occasionally reported.
Allylamines (e.g., Terbinafine):
- Liver issues: Changes in liver function tests and, rarely, serious liver damage.
- Dermatological reactions: Rashes and, more rarely, psoriasis exacerbation or new onset.
- Gastrointestinal distress: Common effects include stomach upset and diarrhea.
- Taste disturbances: Some patients report a temporary or permanent change or loss of taste.
Other Agents:
- Flucytosine: This can cause bone marrow suppression, leading to reduced white blood cells, red blood cells, and platelets, which increases the risk of infections and bleeding. Gastrointestinal upset and liver toxicity are also potential risks.
- Griseofulvin: This may lead to headaches, fatigue, digestive discomfort, and in rare cases, severe allergic reactions.
List of common antifungal medication
Antifungal medications are used to treat a variety of fungal infections, ranging from superficial such as skin or nail infections to deep systemic infections. Below is a list of some commonly prescribed antifungal medications, grouped by their type and typical usage:
Azoles:
- Fluconazole (Diflucan): Commonly used for yeast infections, including thrush and candidiasis, as well as systemic infections.
- Itraconazole (Sporanox): Effective against nail fungus, skin infections, and some systemic infections.
- Ketoconazole (Nizoral): Used primarily for skin infections such as athlete’s foot and dandruff, though now less commonly prescribed for systemic infections due to side effects.
- Clotrimazole (Lotrimin): Widely used for dermatophyte infections, such as athlete’s foot and jock itch, as well as vaginal yeast infections.
- Miconazole (Monistat): Commonly used for vaginal yeast infections and skin infections.
Polyenes:
- Amphotericin B: Used for serious systemic fungal infections and is known for its broad-spectrum efficacy.
- Nystatin: Typically used in the treatment of oral thrush and intestinal candidiasis.
Echinocandins:
- Caspofungin (Cancidas): Used for the treatment of invasive candidiasis and as salvage therapy for invasive aspergillosis.
- Micafungin (Mycamine): Used for the treatment of candidemia, esophageal candidiasis, and prophylaxis against Candida infections in hematopoietic stem cell transplant recipients.
- Anidulafungin (Eraxis): Effective for candidemia and other forms of Candida infections, including intra-abdominal abscesses and peritonitis.
Allylamines:
- Terbinafine (Lamisil): Commonly prescribed for nail fungus (onychomycosis) and scalp infections.
- Naftifine (Naftin): Used primarily for skin infections like athlete’s foot.
Others:
- Griseofulvin (Gris-PEG): Used for scalp, skin, and nail infections caused by dermatophytes. It is one of the older treatments for ringworm.
- Flucytosine (Ancobon): Often used in combination with other antifungals for treating serious infections like cryptococcal meningitis.
- Tolnaftate (Tinactin): Widely used as a cream for treating athlete’s foot, jock itch, and ringworm.
Many antifungals are available in creams, lotions, and sprays for topical use on the skin or mucous membranes, including butoconazole, econazole, and ciclopirox, which are effective for treating local infections without the systemic effects associated with oral medications.
How can DrHouse help?
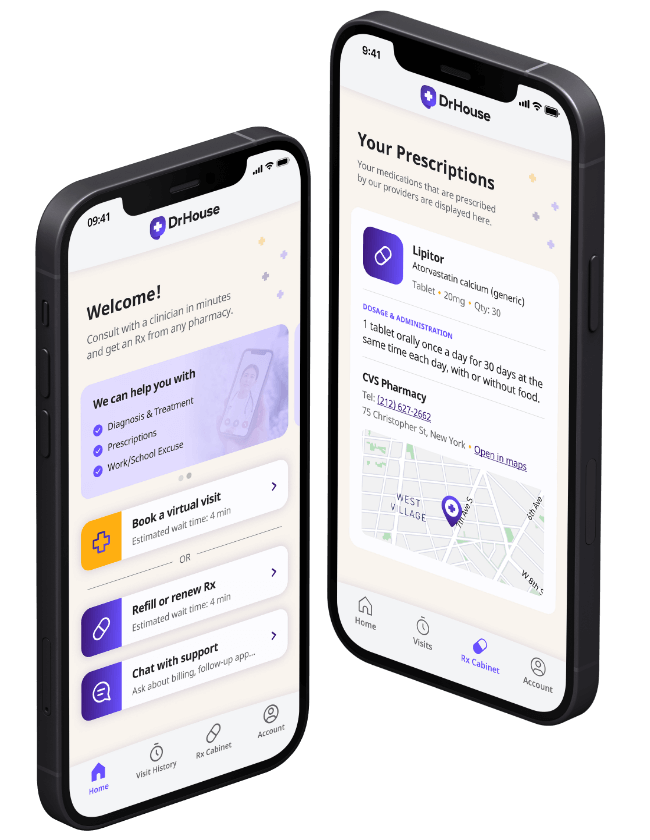
DrHouse offers a convenient telehealth service that allows patients to consult with healthcare professionals from the comfort of their own homes. Our platform supports a wide range of conditions, including fungal infections that may require antifungal medications.
Patients can easily book virtual consultations with experienced providers who can assess their symptoms, discuss potential treatment options, and prescribe medications online when appropriate.
The DrHouse app further enhances this experience by providing a user-friendly interface for managing appointments, accessing health information, and receiving prescriptions directly to their chosen pharmacy.
Here are some ways that DrHouse can help you:
- Convenient access: Patients can schedule virtual consultations at their convenience, avoiding the need to travel to a clinic.
- Expert consultations: Access to qualified healthcare professionals who can provide specialized advice and treatment for fungal infections and other health issues.
- Tailored treatment plans: Providers can develop personalized treatment plans based on individual patient needs and medical histories.
- Prescription services: The platform facilitates the prescribing of necessary antifungal medications, which can be sent directly to the patient’s preferred pharmacy.
- Continuity of care: DrHouse allows for follow-up consultations to monitor the patient’s progress and adjust treatment as needed.
- Privacy and comfort: Patients can seek treatment from the comfort of their home, ensuring privacy and reducing anxiety often associated with medical visits.
- 24/7 access: Our platform is available 24 hours a day, 7 days a week, making it easier for patients to receive care when they need it.
Don’t let a fungal infection disrupt your life. Consult with DrHouse today and get the treatment you need quickly and conveniently.
Download our app today and take control of your health!
Frequently asked questions (FAQs)
Can I get an online prescription antifungals from DrHouse?
Yes, if deemed appropriate by the healthcare provider during the virtual consultation, they can prescribe antifungal medication and send it directly to your preferred pharmacy.
How long does it take to receive my prescription?
It takes around 15 minutes to see an online doctor and receive a prescription, depending on the patient’s individual circumstances.
Related services
Explore more of our services tailored to your needs and discover additional ways we can support your healthcare needs.
Frequently asked questions