Yeast Infection Treatment Online
Get fast, effective treatment for yeast infections online with DrHouse. Connect 24/7 with a virtual doctor for personalized care and prescriptions.
Available in 50 states. Insurance accepted.
Fast
virtual visits
24/7 care
assistants
Prescriptions
as needed



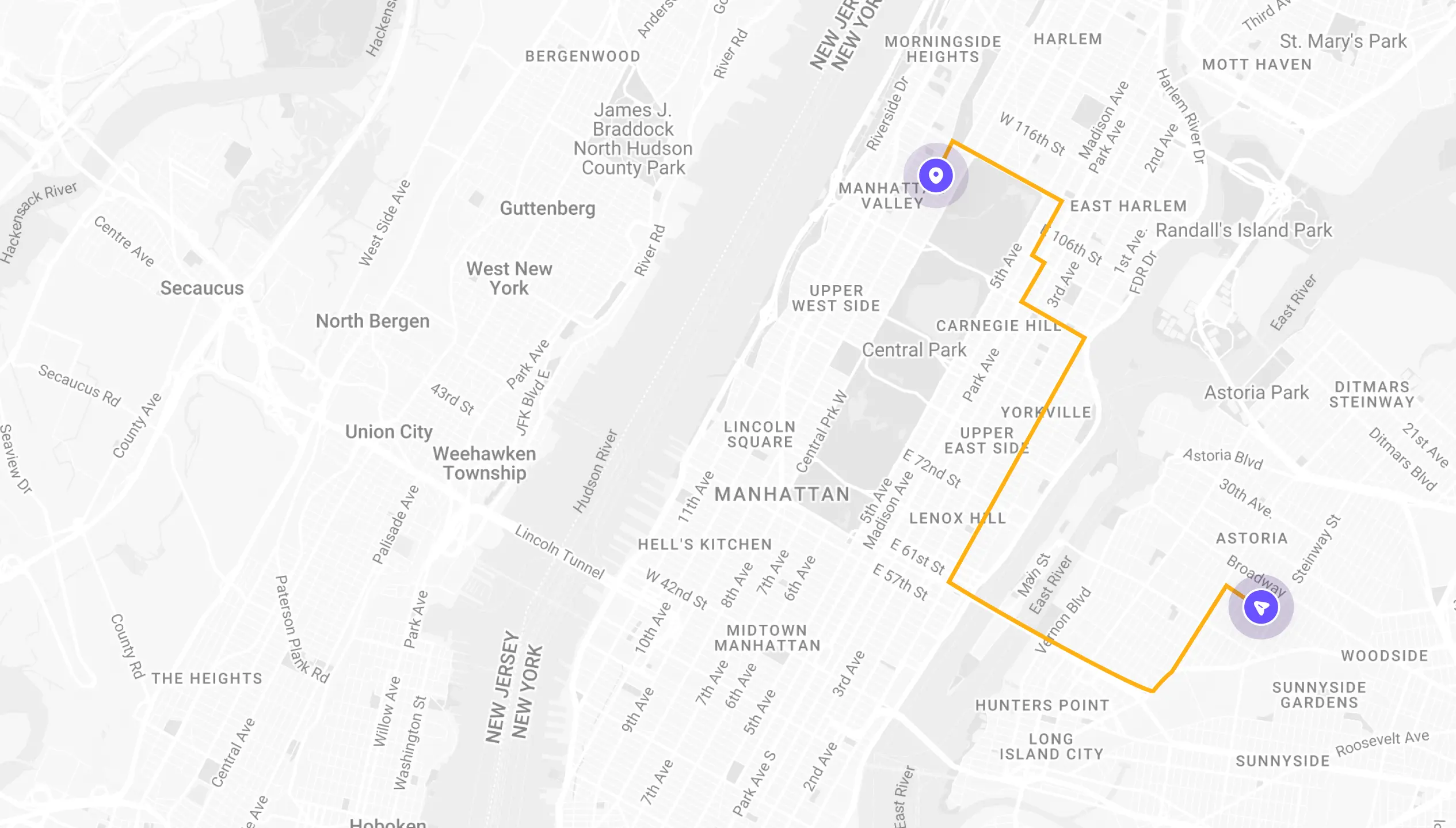
See If Delivery Is Available Near You
Delivery Not Available
Enter your ZIP code to check if prescription delivery is available in your area and how soon your meds could arrive.
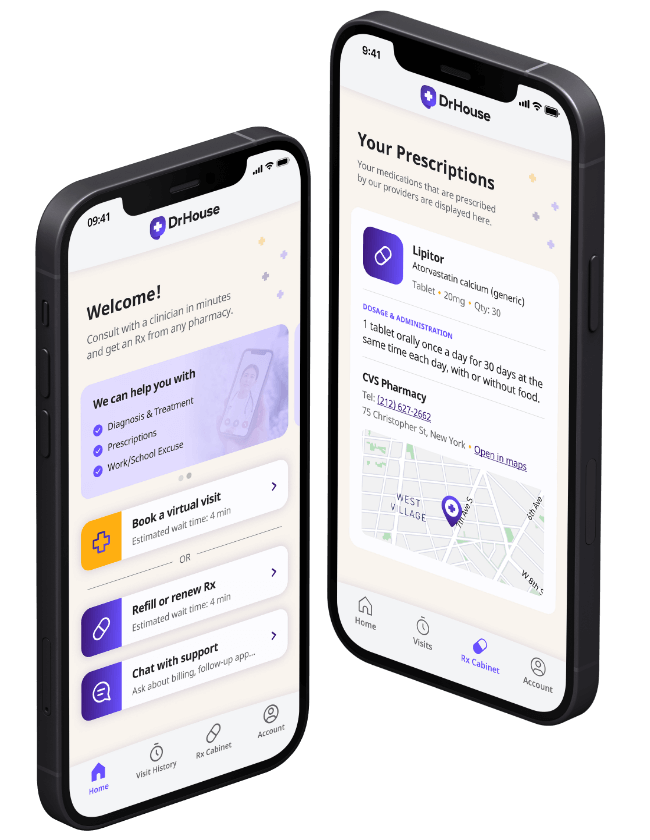
How to get started
Choose your doctor, start a virtual visit, and have your prescriptions sent to your preferred pharmacy for pickup — all in just a few easy steps.
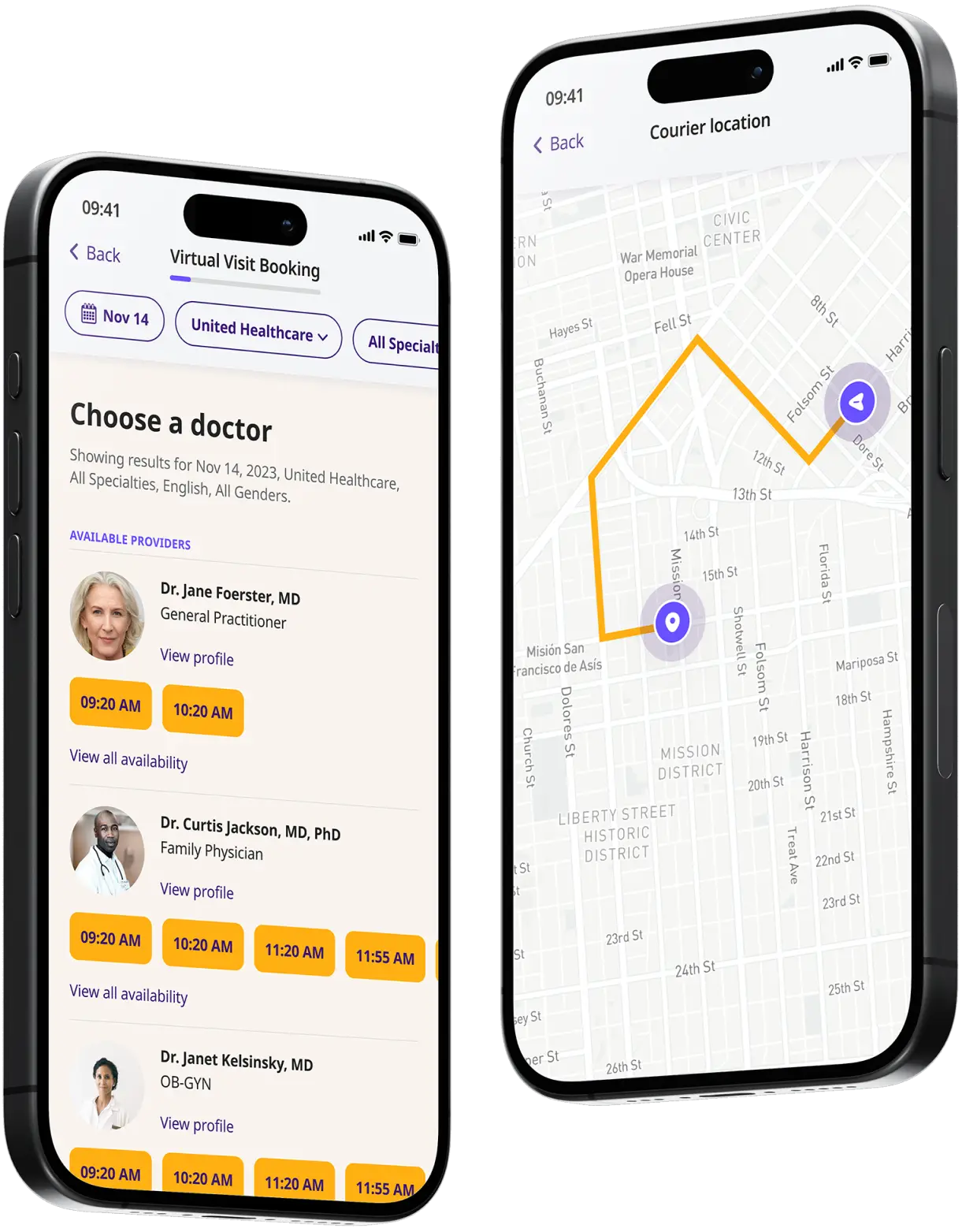
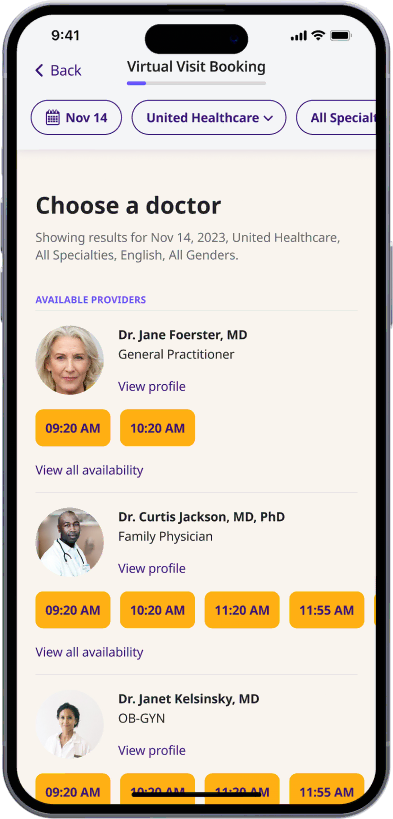
Choose a doctor
Choose a physician by availability, specialty, ratings, and more.
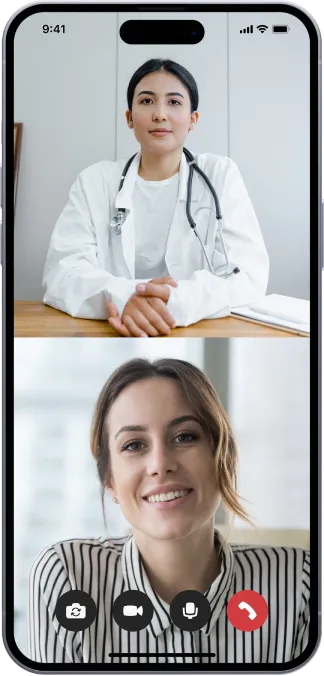
Start a video call
Get connected with a doctor anytime, anywhere.
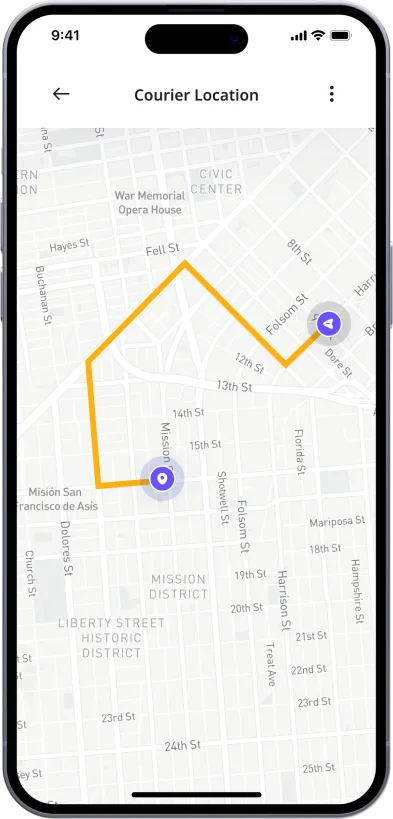
1-Hour Rx Delivery
Your prescription delivered to your door in 1 hour or less.
Available in 50 states. Insurance accepted.
One-Time
Physician Visit
One-time visit with a physician for diagnosis, treatment, Rx, labs, referrals, and doctor’s notes.
Accepted Insurances
See why people turn to DrHouse...
As seen in

Online Yeast Infection Treatment
What Is a Yeast Infection?
A yeast infection is a common type of fungal infection. The scientific name for the fungus that causes yeast infections is Candida. There are more than 20 different species of Candida, but the most common one is Candida albicans. Candida albicans is often found in the gut, mouth, and skin. It’s a normally harmless fungus but can cause an infection if it grows out of control.
Yeast infections can happen anywhere on the body, but most often occurs in warm, moist areas like the digestive tract, mouth, or vagina. When the conditions are right, Candida can multiply quickly and cause an infection.
Yeast infections can happen to anyone, but they’re more common in women. About three out of four women will have at least one vaginal yeast infection in their lifetime. Men can get yeast infections, too, but it’s much less common.
Yeast Infection Symptoms
Yeast infection symptoms can vary depending on where the infection is located on the body. However, there are some common signs to look out for, including:
- Itching and burning sensations in and around the affected area
- Redness, swelling, and inflammation of the skin
- A rash or blisters on the skin
- Discharge from the affected area that is thick and white, similar to cottage cheese
- Pain or discomfort during sexual intercourse
- Soreness in your vagina
If you experience any of these symptoms, it’s important to see your doctor so they can confirm the diagnosis and prescribe treatment.
What Causes Yeast Infections?
There are many different things that can cause a yeast infection. Most yeast infections are caused by a type of fungus called Candida Albicans. This fungus is normally found in small numbers on the skin and in the mouth, gut, and vagina. However, if the balance of bacteria and fungi in the body gets out of whack, the fungus can grow out of control and cause an infection.
There are a number of things that can upset the delicate balance of bacteria and fungi in the body and lead to a yeast infection. For instance, taking antibiotics kills both good and bad bacteria, which can allow Candida to flourish. Diabetes can also cause higher than normal levels of sugar in the blood, which yeast loves to feed on. And pregnant women often have higher levels of estrogen, which can promote the growth of yeast.
Common causes of yeast infection are:
- Taking antibiotics
- Pregnancy
- Diabetes
- Stress
- Hormonal imbalances
- A weak immune system
- Poor diet
- Wearing tight or wet clothing
- And other medical conditions (cancer, aids and etc.)
How to Treat a Yeast Infection?
There are a number of ways to treat a yeast infection, depending on the severity of the infection. For mild yeast infections, over-the-counter antifungal creams or suppositories can be effective. These treatments typically contain an active ingredient such as clotrimazole or miconazole, which helps to kill the yeast that is causing the infection.
For more severe yeast infections, oral antifungal medication may be necessary. This type of treatment is typically taken for two weeks, and it is important to complete the full course of medication even if the symptoms go away.
How Can DrHouse Help You Treat Your Yeast Infection?
If you’re looking for a quick and easy way to treat your yeast infection, DrHouse can help. We provide online diagnosis and treatment for yeast infections, and our online doctors can help you get the relief you need.
With DrHouse, you can start an online doctor visit from the comfort of your own home. Just sign up, and you’ll be able to video chat with one of our online doctors in minutes. We can diagnose and treat your yeast infection online and prescribe medication if needed.
The content on this page has been medically reviewed for accuracy and comprehensiveness by Amy Dougherty, FNP-BC, AGAC
Related services
Explore more of our services tailored to your needs and discover additional ways we can support your healthcare needs.
Frequently asked questions