Get a Prescription for Antibiotics Online 24/7
Get antibiotics prescribed online - manage bacterial infections with a virtual doctor visit for quick diagnosis and treatment.
Available in 50 states. Insurance accepted.
Fast
virtual visits
24/7 care
assistants
Prescriptions
as needed



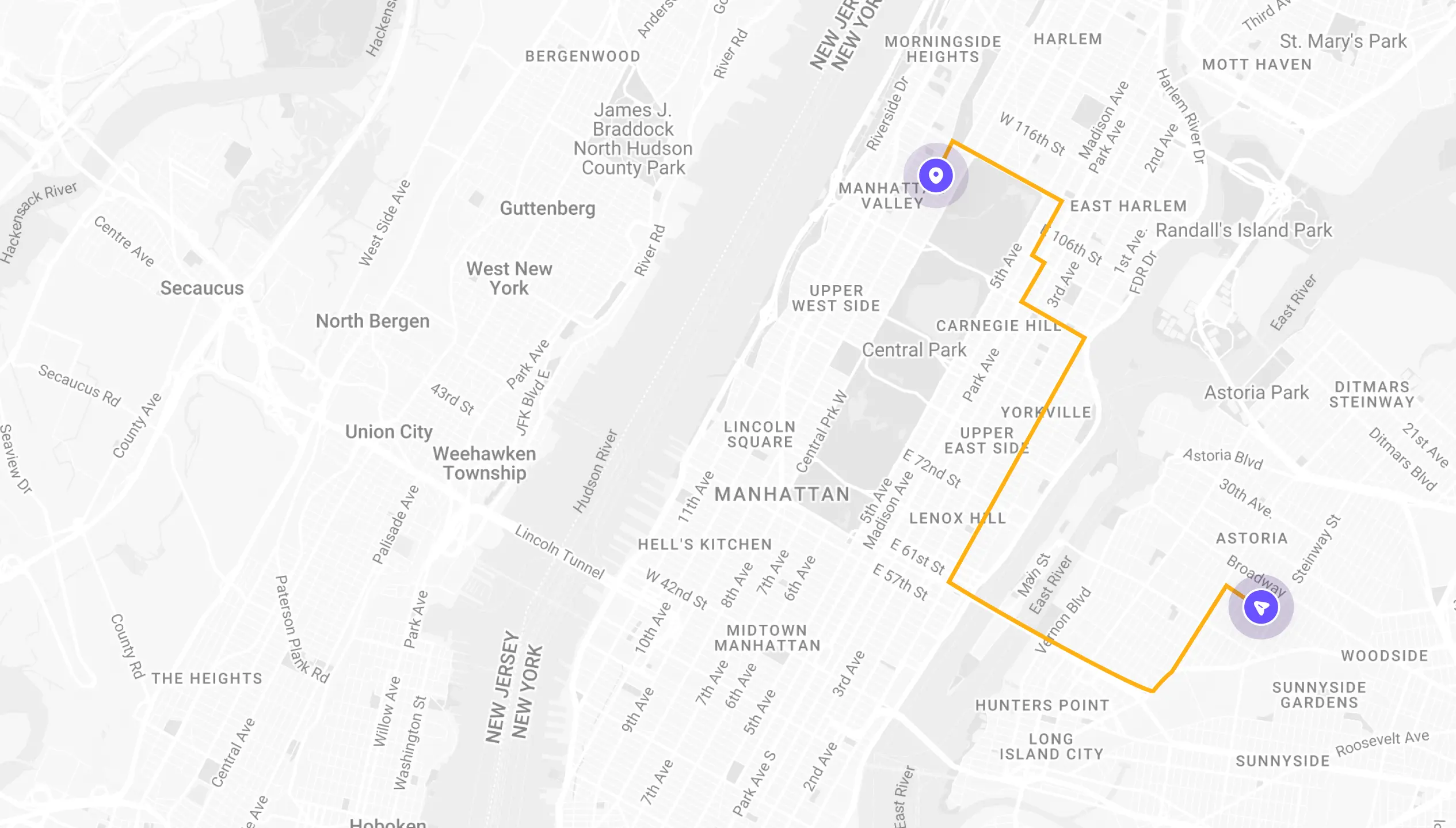
See If Delivery Is Available Near You
Delivery Not Available
Enter your ZIP code to check if prescription delivery is available in your area and how soon your meds could arrive.
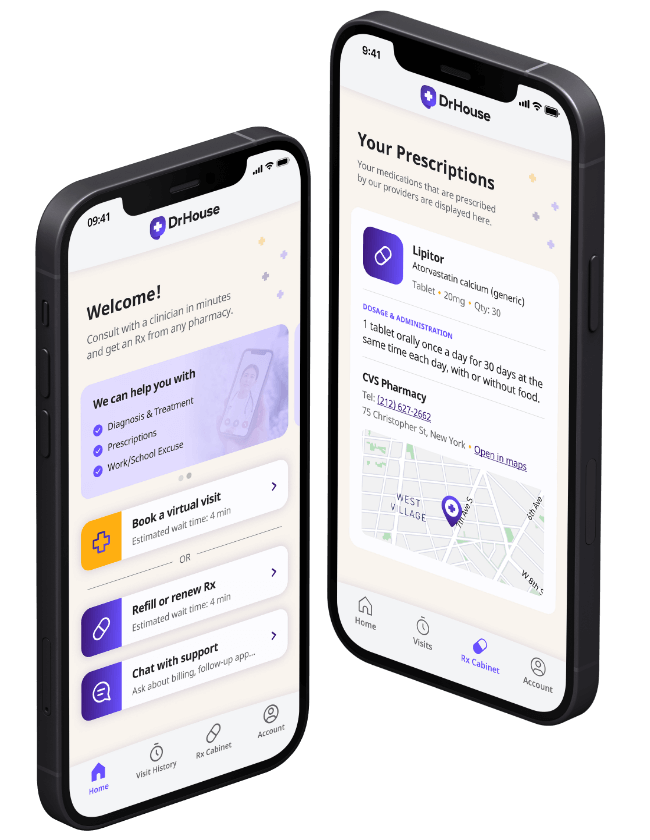
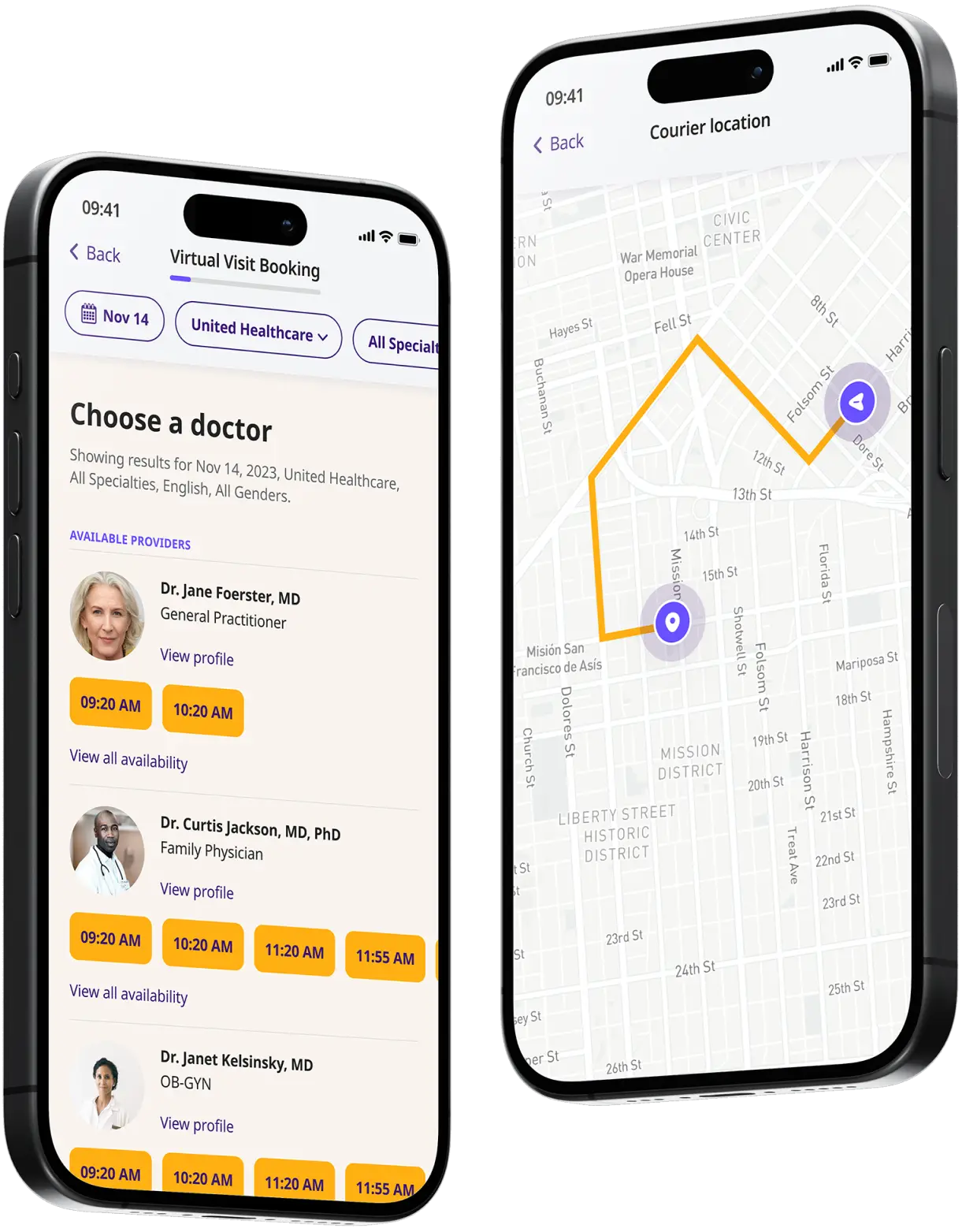
How to get started
Choose your doctor, start a virtual visit, and have your prescriptions sent to your preferred pharmacy for pickup — all in just a few easy steps.
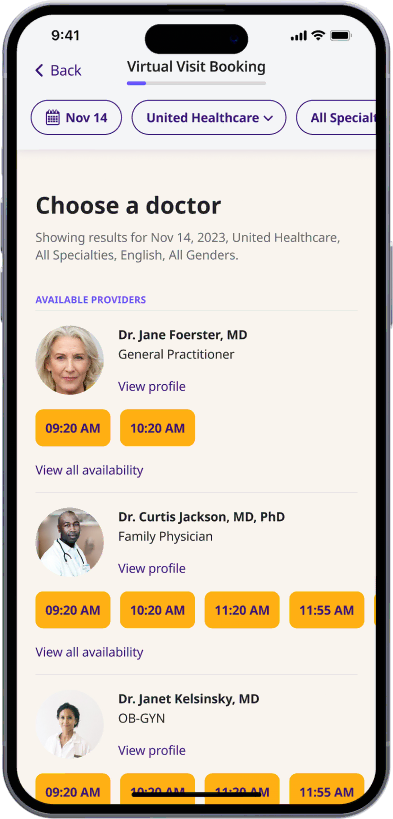
Choose a doctor
Choose a physician by availability, specialty, ratings, and more.
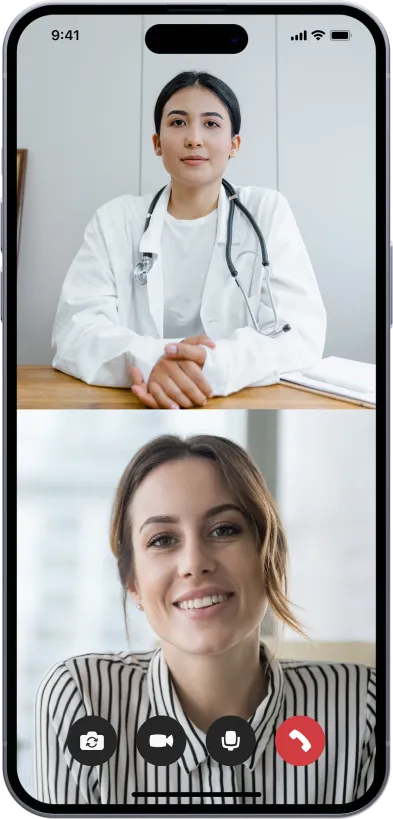
Start a video call
Get connected with a doctor anytime, anywhere.
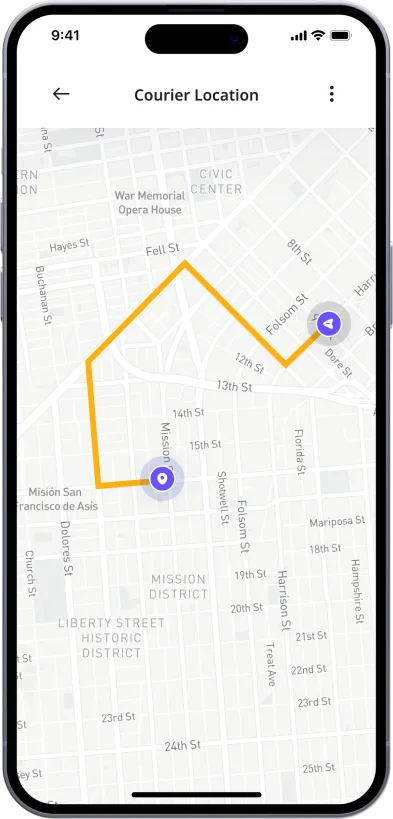
1-Hour Rx Delivery
Your prescription delivered to your door in 1 hour or less.
Available in 50 states. Insurance accepted.
One-Time
Physician Visit
One-time visit with a physician for diagnosis, treatment, Rx, labs, referrals, and doctor’s notes.
Accepted Insurances
See why people turn to DrHouse...
As seen in

Antibiotics
Antibiotics are a class of medications that kill bacteria in the body. Most are taken orally, though some are given intravenously, usually after surgery or in life-threatening situations, such as sepsis.
Medics used the first antibiotic, salvarsan, in 1910, though it was only partially effective. Later, Bayer bacteriologist Gerhard Domagk discovered sulfonamide antibiotics that were more effective against a broad spectrum of microbes in the clinic. They are still in use today.
However, it was only with Alexander Fleming’s 1928 discovery of penicillin that antibiotic usage became mainstream in clinical practice. He and colleagues at Oxford, UK, discovered that the molecule had a molecular structure that could disrupt bacterial cell function.
The golden age of antibiotic discovery came in the middle of the twentieth century, from around 1940 to 1960. Once scientists understood the principle that natural and synthetic compounds could kill bacteria, the race was on to find more.
Early on, the discovery of new antibiotic classes was easy. Researchers and clinicians introduced tetracyclines (1948), macrolides, such as erythromycin (1952), and pyridinamides, such as isoniazid (1952), to clinical practice. However, the discovery of new antibiotics slowed significantly thereafter.
Today, the concern is that antibiotics are losing their effectiveness. Bacteria are evolving to counter the mechanisms that antibiotics use to kill them, leading to the rise of multi-drug-resistant infections.
How Do Antibiotics Work?
Antibiotics work in different ways. Penicillin, for instance, inhibits the production of bacterial cell wall proteins, making them fragile and leaky. When walls burst open, it makes it easier for the immune system to invade and destroy the remaining cell material.
Sulfonamides work differently. They prevent folate synthesis in bacteria, an essential biological process, by inhibiting the enzyme, dihydropteroate synthetase.
Another class of antibiotics, nitrofurans (often used as an antibiotic of last resort) cause DNA damage, making it harder for bacteria to replicate. Similarly, antibiotics prescribed for urinary tract infections, such as ciprofloxacin, inhibit various enzymes required for DNA synthesis.
Tetracyclines, often prescribed for tooth infections and acne, inhibit protein synthesis. Antibiotic compounds enter bacteria cells and then prevent them from producing the compounds they need to build cell structures and replicate.
What are antibiotics Prescribed For?
Physicians prescribe antibiotics for bacterial infections. They do not prescribe them for viral infections because viruses use a different chemistry to spread and replicate. Because of this, they have no effect on the common cold, flu, sore throat, or cough.
Over-prescription of antibiotics increases the risk of microbial resistance, putting future patients at risk. Therefore, physicians usually only prescribe them for serious bacterial infections that the body cannot eliminate by itself. However, some doctors still use them for cosmetic issues, such as acne.
Examples of necessary antibiotic online prescriptions include:
- Sepsis
- Urinary tract infections
- Post-surgery wound infection prevention
- Tuberculosis
- Periodontitis
- Pneumonia
- Strep throat infections
- Whooping cough
- Middle ear infections
- Some sinus infections
Antibiotics either kill bacteria that cause these conditions directly or prevent them from replicating, allowing the immune system to work more effectively.
What Are Common Side Effects of Antibiotics?
While antibiotics kill dangerous bacteria, they can have some off-target effects. Most oral antibiotics, for instance, kill healthy gut bacteria. Because of this, many patients experience nausea, diarrhea, vomiting, and loss of appetite. Antibiotics can also preferentially kill some gut bacteria while allowing others to survive. Overgrowth of certain species can cause abdominal pain, bloating, and indigestion.
Antibiotics can also produce allergic reactions in some patients. Symptoms can range from mild rashes to life-threatening anaphylaxis (an inability to breathe).
Antibiotics have these effects because they contain compounds that confuse the immune system, causing it to believe that the body is under serious threat. The types of antibiotics most likely to cause allergic reactions are amoxicillin, penicillin, tetracyclines, and ampicillin.
Around one in fifteen people has an allergic reaction to antibiotics. Therefore, doctors may perform allergy tests before prescribing them.
What are the most common antibiotics prescribed?
The most commonly prescribed antibiotics combat the diseases that people get most often, such as urinary tract infections and periodontitis. According to the CDC, amoxicillin sits at the top of the list, with 171 prescriptions per 1,000 people per year, followed closely by azithromycin at 144 prescriptions per 1,000 people per year, and amoxicillin/clavulanic acid at 79 prescriptions per 1,000 people per year.
Physicians typically use these antibiotics as a first line of defense to see if they work against common infections. If they are ineffective, they will then move on to lesser-used second or third-line drugs. Amoxicillin is the most prescribed because patients tolerate it well and side effects tend to be minor. Less-used antibiotics, such as nitrofurantoin, are more effective (because there is less microbial resistance to them), but side effects can be more severe.
The content on this page has been medically reviewed for accuracy and comprehensiveness by Amy Dougherty, FNP-BC, AGAC
Related services
Explore more of our services tailored to your needs and discover additional ways we can support your healthcare needs.
Frequently asked questions